Related Research Articles

A vaccine is a biological preparation that provides active acquired immunity to a particular infectious disease. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins. The agent stimulates the body's immune system to recognize the agent as a threat, destroy it, and to further recognize and destroy any of the microorganisms associated with that agent that it may encounter in the future. Vaccines can be prophylactic, or therapeutic. Some vaccines offer full sterilizing immunity, in which infection is prevented completely.

Virology is the scientific study of viruses – submicroscopic, parasitic organisms of genetic material contained in a protein coat – and virus-like agents. It focuses on the following aspects of viruses: their structure, classification and evolution, their ways to infect and exploit host cells for reproduction, their interaction with host organism physiology and immunity, the diseases they cause, the techniques to isolate and culture them, and their use in research and therapy. Virology is a subfield of microbiology.

Vaccinia virus is a large, complex, enveloped virus belonging to the poxvirus family. It has a linear, double-stranded DNA genome approximately 190 kbp in length, which encodes approximately 250 genes. The dimensions of the virion are roughly 360 × 270 × 250 nm, with a mass of approximately 5–10 fg. The vaccinia virus is the source of the modern smallpox vaccine, which the World Health Organisation used to eradicate smallpox in a global vaccination campaign in 1958–1977. Although smallpox no longer exists in the wild, vaccinia virus is still studied widely by scientists as a tool for gene therapy and genetic engineering.
Serial passage is the process of growing bacteria or a virus in iterations. For instance, a virus may be grown in one environment, and then a portion of that virus population can be removed and put into a new environment. This process is repeated with as many stages as desired, and then the final product is studied, often in comparison with the original virus.

Stanley Alan Plotkin is an American physician who works as a consultant to vaccine manufacturers, such as Sanofi Pasteur, as well as biotechnology firms, non-profits and governments. In the 1960s, he played a pivotal role in discovery of a vaccine against rubella virus while working at Wistar Institute in Philadelphia. Plotkin was a member of Wistar’s active research faculty from 1960 to 1991. Today, in addition to his emeritus appointment at Wistar, he is emeritus professor of Pediatrics at the University of Pennsylvania. His book, Vaccines, is the standard reference on the subject. He is an editor with Clinical and Vaccine Immunology, which is published by the American Society for Microbiology in Washington, D.C.
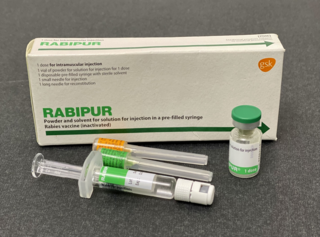
The rabies vaccine is a vaccine used to prevent rabies. There are a number of rabies vaccines available that are both safe and effective. They can be used to prevent rabies before, and, for a period of time, after exposure to the rabies virus, which is commonly caused by a dog bite or a bat bite.

Rabies is a viral disease that causes inflammation of the brain in humans and other mammals. Early symptoms can include fever and tingling at the site of exposure. These symptoms are followed by one or more of the following symptoms: nausea, vomiting, violent movements, uncontrolled excitement, fear of water, an inability to move parts of the body, confusion, and loss of consciousness. Once symptoms appear, the result is virtually always death. The time period between contracting the disease and the start of symptoms is usually one to three months but can vary from less than one week to more than one year. The time depends on the distance the virus must travel along peripheral nerves to reach the central nervous system.

Rabies is a viral zoonotic neuroinvasive disease which causes inflammation in the brain and is usually fatal. Rabies, caused by the rabies virus, primarily infects mammals. In the laboratory it has been found that birds can be infected, as well as cell cultures from birds, reptiles and insects. Animals with rabies suffer deterioration of the brain and tend to behave bizarrely and often aggressively, increasing the chances that they will bite another animal or a person and transmit the disease. Most cases of humans contracting the disease from infected animals are in developing nations. In 2010, an estimated 26,000 people died from rabies, down from 54,000 in 1990.

Tick-borne encephalitis vaccine is a vaccine used to prevent tick-borne encephalitis (TBE). The disease is most common in Central and Eastern Europe, and Northern Asia. More than 87% of people who receive the vaccine develop immunity. It is not useful following the bite of an infected tick. It is given by injection into a muscle.

Rubella vaccine is a vaccine used to prevent rubella. Effectiveness begins about two weeks after a single dose and around 95% of people become immune. Countries with high rates of immunization no longer see cases of rubella or congenital rubella syndrome. When there is a low level of childhood immunization in a population it is possible for rates of congenital rubella to increase as more women make it to child-bearing age without either vaccination or exposure to the disease. Therefore, it is important for more than 80% of people to be vaccinated. By introducing rubella containing vaccines, rubella has been eradicated in 81 nations, as of mid-2020.
As of 2021, a vaccine against Epstein–Barr virus was not yet available. The virus establishes latent infection and causes infectious mononucleosis. There is also increasingly more evidence that EBV may be a trigger of multiple sclerosis. It is a dual-tropic virus, meaning that it infects two different host cell types — in this case, both B cells and epithelial cells. One challenge is that the Epstein–Barr virus expresses very different proteins during its lytic and its latent phases. Antiviral agents act by inhibiting viral DNA replication, but as of 2016 there was little evidence that they are effective against Epstein–Barr virus, they are expensive, they risk causing resistance to antiviral agents, and can cause unpleasant side effects.
A subunit vaccine is a vaccine that contains purified parts of the pathogen that are antigenic, or necessary to elicit a protective immune response. A "subunit" vaccine doesn't contain the whole pathogen, unlike live attenuated or inactivated vaccine, but contains only the antigenic parts such as proteins, polysaccharides or peptides. Because the vaccine doesn't contain "live" components of the pathogen, there is no risk of introducing the disease, and is safer and more stable than vaccine containing whole pathogens. Other advantages include being well-established technology and being suitable for immunocompromised individuals. Disadvantages include being relatively complex to manufacture compared to some vaccines, possibly requiring adjuvants and booster shots, and requiring time to examine which antigenic combinations may work best.

An inactivated vaccine is a vaccine consisting of virus particles, bacteria, or other pathogens that have been grown in culture and then killed to destroy disease-producing capacity. In contrast, live vaccines use pathogens that are still alive. Pathogens for inactivated vaccines are grown under controlled conditions and are killed as a means to reduce infectivity and thus prevent infection from the vaccine.
Peptide-based synthetic vaccines, also called epitope vaccines, are subunit vaccines made from peptides. The peptides mimic the epitopes of the antigen that triggers direct or potent immune responses. Peptide vaccines can not only induce protection against infectious pathogens and non-infectious diseases but also be utilized as therapeutic cancer vaccines, where peptides from tumor-associated antigens are used to induce an effective anti-tumor T-cell response.
Dengue vaccine is a vaccine used to prevent dengue fever in humans. Development of dengue vaccines began in the 1920s, but was hindered by the need to create immunity against all four dengue serotypes.

Ebola vaccines are vaccines either approved or in development to prevent Ebola. The first vaccine to be approved in the United States was rVSV-ZEBOV in December 2019. It had been used extensively in the Kivu Ebola epidemic under a compassionate use protocol. During the early 21st century, several vaccine candidates displayed efficacy to protect nonhuman primates against lethal infection.
A Zika virus vaccine is designed to prevent the symptoms and complications of Zika virus infection in humans. As Zika virus infection of pregnant women may result in congenital defects in the newborn, the vaccine will attempt to protect against congenital Zika syndrome during the current or any future outbreak. As of April 2019, no vaccines have been approved for clinical use, however a number of vaccines are currently in clinical trials. The goal of a Zika virus vaccine is to produce specific antibodies against the Zika virus to prevent infection and severe disease. The challenges in developing a safe and effective vaccine include limiting side effects such as Guillain-Barré syndrome, a potential consequence of Zika virus infection. Additionally, as dengue virus is closely related to Zika virus, the vaccine needs to minimize the possibility of antibody-dependent enhancement of dengue virus infection.

Dame Sarah Catherine Gilbert is a British vaccinologist who is a Professor of Vaccinology at the University of Oxford and co-founder of Vaccitech. Gilbert specialises in the development of vaccines against influenza and emerging viral pathogens. She led the development and testing of the universal flu vaccine, which underwent clinical trials in 2011. On New Year's Day 2020 Gilbert read on ProMED-mail about four people in China suffering from a strange pneumonia of unknown cause, in Wuhan, China. Within two weeks a vaccine had been designed at Oxford against the new pathogen. On 30 December 2020, the Oxford–AstraZeneca COVID-19 vaccine she co-developed with the Oxford Vaccine Group was approved for use in the United Kingdom. As of January 2022 more than 2.5 billion doses of the vaccine have been released to more than 170 countries worldwide.
A nucleoside-modified messenger RNA (modRNA) is a synthetic messenger RNA (mRNA) in which some nucleosides are replaced by other naturally modified nucleosides or by synthetic nucleoside analogues. modRNA is used to induce the production of a desired protein in certain cells. An important application is the development of mRNA vaccines, of which the first authorized were COVID-19 vaccines.

A viral vector vaccine is a vaccine that uses a viral vector to deliver genetic material coding for a desired antigen into the recipient's host cells. As of April 2021, six viral vector vaccines have been authorized for use in humans in at least one country: four COVID-19 vaccines and two Ebola vaccines.
References
- ↑ Keller H, Glueck R, Wegmann A et al. Immunogenicity of a New, Highly Purified, Highly Concentrated Duck Embryo Rabies Vaccine. Schweiz med Wschr 1984; 114:648-653
- ↑ Glueck R, Wegmann A, Germanier R et al. A New, Highly Immunogenic Duck Embryo Rabies Vaccine. The Lancet 1984; April 14: 844.
- ↑ Centers for Disease Control Morbidity and Mortality Weekly Report. Atlanta. January 08, 1999 /48(RR-1);1-21