Related Research Articles

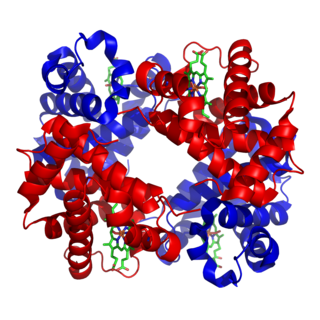
Red blood cells (RBCs), referred to as erythrocytes in academia and medical publishing, also known as red cells, erythroid cells, and rarely haematids, are the most common type of blood cell and the vertebrate's principal means of delivering oxygen to the body tissues—via blood flow through the circulatory system. Erythrocytes take up oxygen in the lungs, or in fish the gills, and release it into tissues while squeezing through the body's capillaries.
Hemolysis or haemolysis, also known by several other names, is the rupturing (lysis) of red blood cells (erythrocytes) and the release of their contents (cytoplasm) into surrounding fluid. Hemolysis may occur in vivo or in vitro.

Anemia or anaemia is a blood disorder in which the blood has a reduced ability to carry oxygen. This can be due to a lower than normal number of red blood cells, a reduction in the amount of hemoglobin available for oxygen transport, or abnormalities in hemoglobin that impair its function.

Spherocytosis is the presence of spherocytes in the blood, i.e. erythrocytes that are sphere-shaped rather than bi-concave disk shaped as normal. Spherocytes are found in all hemolytic anemias to some degree. Hereditary spherocytosis and autoimmune hemolytic anemia are characterized by having only spherocytes.

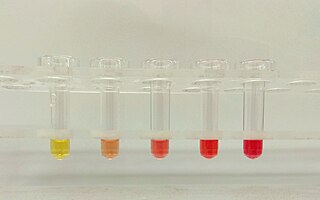
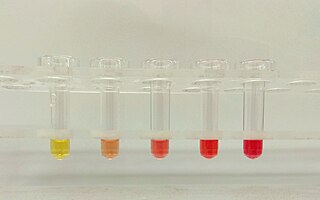
Hereditary spherocytosis (HS) is a congenital hemolytic disorder wherein a genetic mutation coding for a structural membrane protein phenotype causes the red blood cells to be sphere-shaped (spherocytosis), rather than the normal biconcave disk shape. This abnormal shape interferes with the cells' ability to flex during blood circulation, and also makes them more prone to rupture under osmotic stress, mechanical stress, or both. Cells with the dysfunctional proteins are degraded in the spleen, which leads to a shortage of erythrocytes and results in hemolytic anemia.

Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.
The mean corpuscular hemoglobin concentration (MCHC) is a measure of the concentration of hemoglobin in a given volume of packed red blood cell.
The direct and indirect Coombs tests, also known as antiglobulin test (AGT), are blood tests used in immunohematology. The direct Coombs test detects antibodies that are stuck to the surface of the red blood cells. Since these antibodies sometimes destroy red blood cells they can cause anemia; this test can help clarify the condition. The indirect Coombs test detects antibodies that are floating freely in the blood. These antibodies could act against certain red blood cells; the test can be carried out to diagnose reactions to a blood transfusion.

Reticulocytosis is a laboratory finding in which the number of reticulocytes in the bloodstream is elevated. Reticulocytes account for approximately 0.5% to 2.5% of the total red blood cells in healthy adults and 2% to 6% in infants, but in reticulocytosis, this percentage rises. Reticulocytes are produced in the bone marrow and then released into the bloodstream, where they mature into fully developed red blood cells between 1-2 days. Reticulocytosis often reflects the body’s response to conditions rather than an independent disease process and can arise from a variety of causes such as blood loss or anemia.

Codocytes, also known as target cells, are red blood cells that have the appearance of a shooting target with a bullseye. In optical microscopy these cells appear to have a dark center surrounded by a white ring, followed by dark outer (peripheral) second ring containing a band of hemoglobin. However, in electron microscopy they appear very thin and bell shaped. Because of their thinness they are referred to as leptocytes. On routine smear morphology, some people like to make a distinction between leptocytes and codocytes- suggesting that in leptocytes the central spot is not completely detached from the peripheral ring, i.e. the pallor is in a C shape rather than a full ring.

Hereditary elliptocytosis, also known as ovalocytosis, is an inherited blood disorder in which an abnormally large number of the person's red blood cells are elliptical rather than the typical biconcave disc shape. Such morphologically distinctive erythrocytes are sometimes referred to as elliptocytes or ovalocytes. It is one of many red-cell membrane defects. In its severe forms, this disorder predisposes to haemolytic anaemia. Although pathological in humans, elliptocytosis is normal in camelids.

Hereditary stomatocytosis describes a number of inherited, mostly autosomal dominant human conditions which affect the red blood cell and create the appearance of a slit-like area of central pallor (stomatocyte) among erythrocytes on peripheral blood smear. The erythrocytes' cell membranes may abnormally 'leak' sodium and/or potassium ions, causing abnormalities in cell volume. Hereditary stomatocytosis should be distinguished from acquired causes of stomatocytosis, including dilantin toxicity and alcoholism, as well as artifact from the process of preparing peripheral blood smears.

Hereditary pyropoikilocytosis (HPP) is an autosomal recessive form of hemolytic anemia characterized by an abnormal sensitivity of red blood cells to heat and erythrocyte morphology similar to that seen in thermal burns or from prolonged exposure of a healthy patient's blood sample to high ambient temperatures. Patients with HPP tend to experience severe hemolysis and anemia in infancy that gradually improves, evolving toward typical elliptocytosis later in life. However, the hemolysis can lead to rapid sequestration and destruction of red cells. Splenectomy is curative when this occurs.
Autoimmune hemolytic anemia (AIHA) is an autoimmune disorder which occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in circulation (anemia). The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5–10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold-antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
Reticulocytopenia is the medical term for an abnormal decrease in circulating red blood cell precursors (reticulocytes) that can lead to anemia due to resulting low red blood cell (erythrocyte) production. Reticulocytopenia may be an isolated finding or it may not be associated with abnormalities in other hematopoietic cell lineages such as those that produce white blood cells (leukocytes) or platelets (thrombocytes), a decrease in all three of these lineages is referred to as pancytopenia.
Normocytic anemia is a type of anemia and is a common issue that occurs for men and women typically over 85 years old. Its prevalence increases with age, reaching 44 percent in men older than 85 years. The most common type of normocytic anemia is anemia of chronic disease.
Hemolysis or haemolysis, also known by several other names, is the rupturing (lysis) of red blood cells (erythrocytes) and the release of their contents (cytoplasm) into surrounding fluid. Hemolysis may occur in vivo or in vitro.
Drug-induced nonautoimmune hemolytic anemia is a uncommon cause of hemolytic anemia. In drug-induced nonautoimmune hemolytic anemia, red blood cells (RBC) are destroyed from various non-immune mechanisms such as direct oxidative stress from certain drugs. This is in contrast to drug-induced autoimmune hemolytic anemia where certain drugs result in the formation of antibodies against RBCs, resulting in hemolysis.
In hematology, erythrocyte deformability refers to the ability of erythrocytes to change shape under a given level of applied stress without hemolysing (rupturing). This is an important property because erythrocytes must change their shape extensively under the influence of mechanical forces in fluid flow or while passing through microcirculation. The extent and geometry of this shape change can be affected by the mechanical properties of the erythrocytes, the magnitude of the applied forces, and the orientation of erythrocytes with the applied forces. Deformability is an intrinsic cellular property of erythrocytes determined by geometric and material properties of the cell membrane, although as with many measurable properties the ambient conditions may also be relevant factors in any given measurement. No other cells of mammalian organisms have deformability comparable with erythrocytes; furthermore, non-mammalian erythrocytes are not deformable to an extent comparable with mammalian erythrocytes. In human RBCs there are structural supports that aid resilience, which include the cytoskeleton: actin and spectrin that are held together by ankyrin.
Mechanical hemolytic anemia is a form of hemolytic anemia due to mechanically induced damage to red blood cells. Red blood cells, while flexible, may in some circumstances succumb to physical shear and compression. This may result in hemoglobinuria. The damage is induced through repetitive mechanical motions such as prolonged marching and marathon running. Mechanical damage can also be induced through the chronic condition microangiopathic hemolytic anemia or due to prosthetic heart valves.
References
- ↑ Greenaway, Chris (January 31, 2012). "Osmotic fragility test". spherocytosis.info. Archived from the original on June 3, 2012.
- ↑ DE KRETSER AJ, WALDRON HA (1963). "The Mechanical Fragility of the Red Cell in Patients with Lead Poisoning". Br J Ind Med. 20 (4): 316–9. doi:10.1136/oem.20.4.316. PMC 1039189 . PMID 14072624.
- ↑ Rodak, Bernadette F.; et al. (2007). Hematology: clinical principles and applications. Elsevier Health Sciences. p. 291. ISBN 978-1-4160-3006-5.
- ↑ Fischbach, Frances Talaska; Dunning, Marshall Barnett (2008). A manual of laboratory and diagnostic tests (8th ed.). Lippincott Williams & Wilkins. p. 116. ISBN 978-0-7817-7194-8.
- ↑ Greer, John P.; et al., eds. (2008). Wintrobe's clinical hematology. Lippincott Williams & Wilkins. p. 805. ISBN 978-0-7817-6507-7.
- ↑ "How is hereditary spherocytosis (HS) differentiated from hereditary xerocytosis (HX)?". Archived from the original on 2024-07-06. Retrieved 2024-07-06.
- ↑ "Osmotic Fragility is a test for hereditary spherocytosis - ClinLab Navigator". clinlabnavigator.com. Archived from the original on 2013-01-07. Retrieved 2013-03-28.
- ↑ Chen, Hongda; Ye, Datian; Wu, Hongkai; Peng, Fei; Li, Jing; Su, Jing; Li, Lei (2012-07-30). "A microfluidic platform for osmotic fragility test of red blood cells". RSC Advances. 2 (18): 7161–7165. Bibcode:2012RSCAd...2.7161L. doi:10.1039/C2RA20051A.
- 1 2 Gu, Lei; Smith, William A.; Chatzimavroudis, George P. (2005). "Mechanical Fragility Calibration of Red Blood Cells". ASAIO Journal. 51 (3). Ovid Technologies (Wolters Kluwer Health): 194–201. doi:10.1097/01.mat.0000161940.30190.6d. ISSN 1058-2916.
- ↑ "Obsolete and Unreliable Tests and Procedures". aetna.com. Archived from the original on 2014-01-02. Retrieved 2013-03-28.
- ↑ "2021 Clinical Diagnostic Laboratory Fee Schedule" (PDF). Archived (PDF) from the original on 26 February 2024. Retrieved 4 July 2024.
- ↑ Kameneva, Marina V.; Marad, Paul F.; Brugger, James M.; Repko, Brandon M.; Wang, John H.; Moran, John; Borovetz, Harvey S. (2002). "In Vitro Evaluation of Hemolysis and Sublethal Blood Trauma in a Novel Subcutaneous Vascular Access System for Hemodialysis". ASAIO Journal. 48 (1). Ovid Technologies (Wolters Kluwer Health): 34–38. doi:10.1097/00002480-200201000-00008. ISSN 1058-2916.
- ↑ Yazer M. H.; Waters J. H.; Elkin K. R.; Rohrbaugh M. E.; Kameneva M. V. (2008). "A comparison of hemolysis and red cell mechanical fragility in blood collected with different cell salvage suction devices". Transfusion. 48 (6): 1188–1191. doi:10.1111/j.1537-2995.2008.01670.x. PMID 18346016. S2CID 28610759.
- ↑ Raval, J. S.; Waters, J. H.; Seltsam, A.; Scharberg, E. A.; Richter, E.; Daly, A. R.; Kameneva, M. V.; Yazer, M. H. (2010-07-27). "The use of the mechanical fragility test in evaluating sublethal RBC injury during storage". Vox Sanguinis. 99 (4). Wiley: 325–331. doi:10.1111/j.1423-0410.2010.01365.x. ISSN 0042-9007.
- ↑ Baskurt, O.K.; Hardeman, M.R.; Rampling, M.W. (2007). Handbook of Hemorheology and Hemodynamics. Biomedical and Health Research. IOS Press. ISBN 978-1-60750-263-0. Archived from the original on 2024-07-06. Retrieved 2024-07-04.
- ↑ Tarssanen, L. (1976). "Hemolysis by ultrasound. A comparative study of the osmotic and ultrasonic fragility tests". Scandinavian Journal of Haematology. Supplementum. 29: 1–59. ISSN 0080-6722. PMID 1064894.