Vitamin K is a family of structurally similar, fat-soluble vitamers found in foods and marketed as dietary supplements. The human body requires vitamin K for post-synthesis modification of certain proteins that are required for blood coagulation or for controlling binding of calcium in bones and other tissues. The complete synthesis involves final modification of these so-called "Gla proteins" by the enzyme gamma-glutamyl carboxylase that uses vitamin K as a cofactor.

Bleeding, hemorrhage, haemorrhage or blood loss, is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vagina or anus, or through a puncture in the skin. Hypovolemia is a massive decrease in blood volume, and death by excessive loss of blood is referred to as exsanguination. Typically, a healthy person can endure a loss of 10–15% of the total blood volume without serious medical difficulties. The stopping or controlling of bleeding is called hemostasis and is an important part of both first aid and surgery.

Anticoagulants, commonly known as blood thinners, are chemical substances that prevent or reduce coagulation of blood, prolonging the clotting time. Some of them occur naturally in blood-eating animals such as leeches and mosquitoes, where they help keep the bite area unclotted long enough for the animal to obtain some blood. As a class of medications, anticoagulants are used in therapy for thrombotic disorders. Oral anticoagulants (OACs) are taken by many people in pill or tablet form, and various intravenous anticoagulant dosage forms are used in hospitals. Some anticoagulants are used in medical equipment, such as sample tubes, blood transfusion bags, heart–lung machines, and dialysis equipment. One of the first anticoagulants, warfarin, was initially approved as a rodenticide.

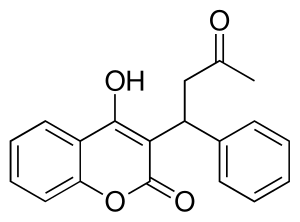
Warfarin is an anticoagulant used as a medication under several brand names including Coumadin. While the drug is described as a "blood thinner", it does not reduce viscosity but rather inhibits coagulation. Accordingly, it is commonly used to prevent blood clots in the circulatory system such as deep vein thrombosis and pulmonary embolism, and to protect against stroke in people who have atrial fibrillation, valvular heart disease, or artificial heart valves. Less commonly, it is used following ST-segment elevation myocardial infarction and orthopedic surgery. It is usually taken by mouth, but may also be administered intravenously.

Antiphospholipid syndrome, or antiphospholipid antibody syndrome, is an autoimmune, hypercoagulable state caused by antiphospholipid antibodies. APS provokes blood clots (thrombosis) in both arteries and veins as well as pregnancy-related complications such as miscarriage, stillbirth, preterm delivery, and severe preeclampsia. Although the exact etiology of APS is still not clear, genetics is believed to play a key role in the development of the disease. The diagnostic criteria require one clinical event and two positive blood test results spaced at least three months apart that detect lupus anticoagulant, anti-apolipoprotein antibodies, or anti-cardiolipin antibodies.

The prothrombin time (PT) – along with its derived measures of prothrombin ratio (PR) and international normalized ratio (INR) – is an assay for evaluating the extrinsic pathway and common pathway of coagulation. This blood test is also called protime INR and PT/INR. They are used to determine the clotting tendency of blood, in such things as the measure of warfarin dosage, liver damage, and vitamin K status. PT measures the following coagulation factors: I (fibrinogen), II (prothrombin), V (proaccelerin), VII (proconvertin), and X.

Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis. Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes. A significant proportion of the population has a detectable thrombophilic abnormality, but most of these develop thrombosis only in the presence of an additional risk factor.

Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.

Renal vein thrombosis (RVT) is the formation of a clot in the vein that drains blood from the kidneys, ultimately leading to a reduction in the drainage of one or both kidneys and the possible migration of the clot to other parts of the body. First described by German pathologist Friedrich Daniel von Recklinghausen in 1861, RVT most commonly affects two subpopulations: newly born infants with blood clotting abnormalities or dehydration and adults with nephrotic syndrome.

Hypoprothrombinemia is a rare blood disorder in which a deficiency in immunoreactive prothrombin, produced in the liver, results in an impaired blood clotting reaction, leading to an increased physiological risk for spontaneous bleeding. This condition can be observed in the gastrointestinal system, cranial vault, and superficial integumentary system, affecting both the male and female population. Prothrombin is a critical protein that is involved in the process of hemostasis, as well as illustrating procoagulant activities. This condition is characterized as an autosomal recessive inheritance congenital coagulation disorder affecting 1 per 2,000,000 of the population, worldwide, but is also attributed as acquired.

Phenprocoumon is a long-acting blood thinner drug to be taken by mouth, and a derivative of coumarin. It acts as a vitamin K antagonist and inhibits blood clotting (coagulation) by blocking synthesis of coagulation factors II, VII, IX and X. It is used for the prophylaxis and treatment of thromboembolic disorders such as heart attacks and pulmonary (lung) embolism. The most common adverse effect is bleeding. The drug interacts with a large number of other medications, including aspirin and St John's Wort. It is the standard coumarin used in Germany, Austria, and other European countries.

Dabigatran, sold under the brand name Pradaxa among others, is an anticoagulant used to treat and prevent blood clots and to prevent stroke in people with atrial fibrillation. Specifically it is used to prevent blood clots following hip or knee replacement and in those with a history of prior clots. It is used as an alternative to warfarin and does not require monitoring by blood tests. In a meta analysis of 7 different studies, there was no benefit of dabigatran over warfarin in preventing ischemic stroke; however, dabigatran were associated with a lower hazard for intracranial bleeding compared with warfarin, but also had a higher risk of gastrointestinal bleeding relative to warfarin. It is taken by mouth.
Hypercoagulability in pregnancy is the propensity of pregnant women to develop thrombosis. Pregnancy itself is a factor of hypercoagulability, as a physiologically adaptive mechanism to prevent post partum bleeding. However, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.

Percutaneous umbilical cord blood sampling (PUBS), also called cordocentesis, fetal blood sampling, or umbilical vein sampling is a diagnostic genetic test that examines blood from the fetal umbilical cord to detect fetal abnormalities. Fetal and maternal blood supply are typically connected in utero with one vein and two arteries to the fetus. The umbilical vein is responsible for delivering oxygen rich blood to the fetus from the mother; the umbilical arteries are responsible for removing oxygen poor blood from the fetus. This allows for the fetus’ tissues to properly perfuse. PUBS provides a means of rapid chromosome analysis and is useful when information cannot be obtained through amniocentesis, chorionic villus sampling, or ultrasound ; this test carries a significant risk of complication and is typically reserved for pregnancies determined to be at high risk for genetic defect. It has been used with mothers with immune thrombocytopenic purpura.

The human gene VKORC1 encodes for the enzyme, Vitamin K epOxide Reductase Complex (VKORC) subunit 1. This enzymatic protein complex is responsible for reducing vitamin K 2,3-epoxide to its active form, which is important for effective clotting (coagulation). In humans, mutations in this gene can be associated with deficiencies in vitamin-K-dependent clotting factors.

Vitamin K antagonists (VKA) are a group of substances that reduce blood clotting by reducing the action of vitamin K. The term "vitamin K antagonist" is technically a misnomer, as the drugs do not directly antagonize the action of vitamin K in the pharmacological sense, but rather the recycling of vitamin K. Vitamin K antagonists (VKAs) have been the mainstay of anticoagulation therapy for more than 50 years.

Vitamin K reactions are adverse side effects that may occur after injection with vitamin K. The liver utilizes vitamin K to produce coagulation factors that help the body form blood clots which prevent excessive bleeding. Vitamin K injections are administered to newborns as a preventative measure to reduce the risk of hemorrhagic disease of the newborn (HDN).
Women should speak to their doctor or healthcare professional before starting or stopping any medications while pregnant. Non-essential drugs and medications should be avoided while pregnant. Tobacco, alcohol, marijuana, and illicit drug use while pregnant may be dangerous for the unborn baby and may lead to severe health problems and/or birth defects. Even small amounts of alcohol, tobacco, and marijuana have not been proven to be safe when taken while pregnant. In some cases, for example, if the mother has epilepsy or diabetes, the risk of stopping a medication may be worse than risks associated with taking the medication while pregnant. The mother's healthcare professional will help make these decisions about the safest way to protect the health of both the mother and unborn child. In addition to medications and substances, some dietary supplements are important for a healthy pregnancy, however, others may cause harm to the unborn child.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.
A pre-existing disease in pregnancy is a disease that is not directly caused by the pregnancy, in contrast to various complications of pregnancy, but which may become worse or be a potential risk to the pregnancy. A major component of this risk can result from necessary use of drugs in pregnancy to manage the disease.