Disease
Damage to the optic nerve typically causes permanent and potentially severe loss of vision, as well as an abnormal pupillary reflex, which is important for the diagnosis of nerve damage.
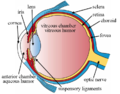
The type of visual field loss will depend on which portions of the optic nerve were damaged. In general, the location of the damage in relation to the optic chiasm (see diagram above) will affect the areas of vision loss. Damage to the optic nerve that is anterior, or in front of the optic chiasm (toward the face) causes loss of vision in the eye on the same side as the damage. Damage at the optic chiasm itself typically causes loss of vision laterally in both visual fields or bitemporal hemianopsia (see image to the right). Such damage may occur with large pituitary tumors, such as pituitary adenoma. Finally, damage to the optic tract, which is posterior to, or behind the chiasm, causes loss of the entire visual field from the side opposite the damage, e.g. if the left optic tract were cut, there would be a loss of vision from the entire right visual field.
Injury to the optic nerve can be the result of congenital or inheritable problems like Leber's hereditary optic neuropathy, glaucoma, trauma, toxicity, inflammation, ischemia, infection (very rarely), or compression from tumors or aneurysms. By far, the three most common injuries to the optic nerve are from glaucoma; optic neuritis, especially in those younger than 50 years of age; and anterior ischemic optic neuropathy, usually in those older than 50.
Glaucoma is a group of diseases involving loss of retinal ganglion cells causing optic neuropathy in a pattern of peripheral vision loss, initially sparing central vision. Glaucoma is frequently associated with increased intraocular pressure that damages the optic nerve as it exits the eyeball. The trabecular meshwork assists the drainage of aqueous humor fluid. The presence of excess aqueous humor, increases IOP, yielding the diagnosis and symptoms of glaucoma. [9]
Optic neuritis is inflammation of the optic nerve. It is associated with a number of diseases, the most notable one being multiple sclerosis. The patient will likely experience varying vision loss and eye pain. The condition tends to be episodic.
Anterior ischemic optic neuropathy is commonly known as a "stroke of the optic nerve" and affects the optic nerve head (where the nerve exits the eyeball). There is usually a sudden loss of blood supply and nutrients to the optic nerve head. Vision loss is typically sudden and most commonly occurs upon waking up in the morning. This condition is most common in diabetic patients 40–70 years old.
Other optic nerve problems are less common. Optic nerve hypoplasia is the underdevelopment of the optic nerve resulting in little to no vision in the affected eye. Tumors, especially those of the pituitary gland, can put pressure on the optic nerve causing various forms of visual loss. Similarly, cerebral aneurysms, a swelling of blood vessel(s), can also affect the nerve. Trauma can cause serious injury to the nerve. Direct optic nerve injury can occur from a penetrating injury to the orbit, but the nerve can also be injured by indirect trauma in which severe head impact or movement stretches or even tears the nerve. [1]
Ophthalmologists and optometrists can detect and diagnose some optic nerve diseases but neuro-ophthalmologists are often best suited to diagnose and treat diseases of the optic nerve. The International Foundation for Optic Nerve Diseases (IFOND) sponsors research and provides information on a variety of optic nerve disorders.