The parasympathetic nervous system (PSNS) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

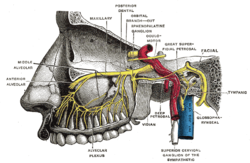
The facial nerve, also known as the seventh cranial nerve, cranial nerve VII, or simply CN VII, is a cranial nerve that emerges from the pons of the brainstem, controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue. The nerve typically travels from the pons through the facial canal in the temporal bone and exits the skull at the stylomastoid foramen. It arises from the brainstem from an area posterior to the cranial nerve VI and anterior to cranial nerve VIII.
Articles related to anatomy include:
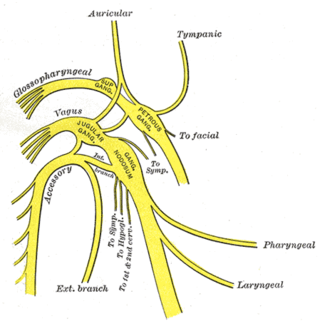
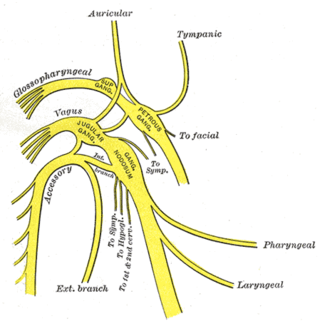
The glossopharyngeal nerve, also known as the ninth cranial nerve, cranial nerve IX, or simply CN IX, is a cranial nerve that exits the brainstem from the sides of the upper medulla, just anterior to the vagus nerve. Being a mixed nerve (sensorimotor), it carries afferent sensory and efferent motor information. The motor division of the glossopharyngeal nerve is derived from the basal plate of the embryonic medulla oblongata, whereas the sensory division originates from the cranial neural crest.
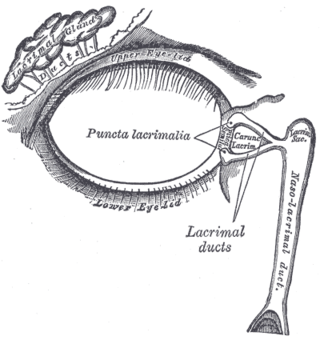
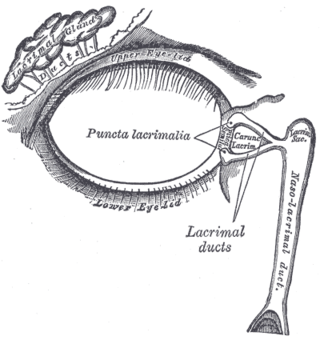
The lacrimal glands are paired exocrine glands, one for each eye, found in most terrestrial vertebrates and some marine mammals, that secrete the aqueous layer of the tear film. In humans, they are situated in the upper lateral region of each orbit, in the lacrimal fossa of the orbit formed by the frontal bone. Inflammation of the lacrimal glands is called dacryoadenitis. The lacrimal gland produces tears which are secreted by the lacrimal ducts, and flow over the ocular surface, and then into canals that connect to the lacrimal sac. From that sac, the tears drain through the lacrimal duct into the nose.

The otic ganglion is a small parasympathetic ganglion located immediately below the foramen ovale in the infratemporal fossa and on the medial surface of the mandibular nerve. It is functionally associated with the glossopharyngeal nerve and innervates the parotid gland for salivation.

The greater petrosal nerve is a nerve of the head mainly containing pre-ganglionic parasympathetic fibres which ultimately synapse in the pterygopalatine ganglion. It branches from the facial nerve and is derived from the parasympathetic part of the nervus intermedius component of CN VII, with its cell bodies located in the superior salivary nucleus. In the connective tissue substance of the foramen lacerum, the greater petrosal nerve unites with the (sympathetic) deep petrosal nerve to form the nerve of the pterygoid canal which proceeds to the pterygopalatine ganglion.

In neuroanatomy, the maxillary nerve (V2) is one of the three branches or divisions of the trigeminal nerve, the fifth (CN V) cranial nerve. It comprises the principal functions of sensation from the maxilla, nasal cavity, sinuses, the palate and subsequently that of the mid-face, and is intermediate, both in position and size, between the ophthalmic nerve and the mandibular nerve.

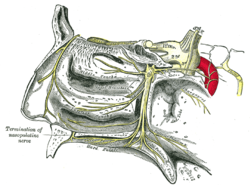
In human anatomy, the pterygopalatine fossa is a fossa in the skull. A human skull contains two pterygopalatine fossae—one on the left side, and another on the right side. Each fossa is a cone-shaped paired depression deep to the infratemporal fossa and posterior to the maxilla on each side of the skull, located between the pterygoid process and the maxillary tuberosity close to the apex of the orbit. It is the indented area medial to the pterygomaxillary fissure leading into the sphenopalatine foramen. It communicates with the nasal and oral cavities, infratemporal fossa, orbit, pharynx, and middle cranial fossa through eight foramina.

The zygomatic nerve is a branch of the maxillary nerve. It arises in the pterygopalatine fossa and enters the orbit through the inferior orbital fissure before dividing into its two terminal branches: the zygomaticotemporal nerve and zygomaticofacial nerve.

The submandibular ganglion is part of the human autonomic nervous system. It is one of four parasympathetic ganglia of the head and neck..

Parasympathetic ganglia are the autonomic ganglia of the parasympathetic nervous system. Most are small terminal ganglia or intramural ganglia, so named because they lie near or within (respectively) the organs they innervate. The exceptions are the four paired parasympathetic ganglia of the head and neck.

The deep petrosal nerve is a post-ganglionic branch of the (sympathetic) internal carotid (nervous) plexus that enters the cranial cavity through the carotid canal, then passes perpendicular to the carotid canal in the cartilaginous substance which fills the foramen lacerum to unite with the (parasympathetic) greater petrosal nerve to form the nerve of pterygoid canal.

The nerve of the pterygoid canal is formed by the union of the (parasympathetic) greater petrosal nerve and (sympathetic) deep petrosal nerve within the cartilaginous substance filling the foramen lacerum. From the foramen lacerum, the nerve of the pterygoid canal passes through the pterygoid canal to reach the pterygopalatine fossa, ending at the pterygopalatine ganglion.

The salivatory nuclei are two parasympathetic general visceral efferent cranial nerve nuclei - the superior salivatory nucleus and the inferior salivatory nucleus - that innervate the salivary glands. Both are located in the pontine tegmentum of the brainstem.

The following outline is provided as an overview of and topical guide to human anatomy:
The autonomic nerve is a small nerve which carries postganglionic sympathetic and parasympathetic neurons from the zygomaticotemporal nerve; a branch of the maxillary nerve, to the lacrimal nerve; a branch of the ophthalmic nerve. These neurons derive from the superior cervical ganglion and the pterygopalatine ganglion respectively. They will travel to the lacrimal gland via the lacrimal nerve. Parasympathetic will induce lacrimation and vice versa.

The following diagram is provided as an overview of and topical guide to the human nervous system:

The ciliary ganglion is a parasympathetic ganglion located just behind the eye in the posterior orbit. Three types of axons enter the ciliary ganglion but only the preganglionic parasympathetic axons synapse there. The entering axons are arranged into three roots of the ciliary ganglion, which join enter the posterior surface of the ganglion.