The autonomic nervous system (ANS), formerly referred to as the vegetative nervous system, is a division of the nervous system that operates internal organs, smooth muscle and glands. The autonomic nervous system is a control system that acts largely unconsciously and regulates bodily functions, such as the heart rate, its force of contraction, digestion, respiratory rate, pupillary response, urination, and sexual arousal. This system is the primary mechanism in control of the fight-or-flight response.

The parasympathetic nervous system (PSNS) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

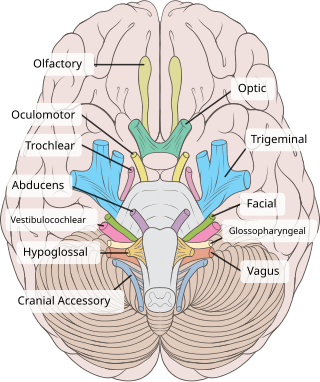
The facial nerve, also known as the seventh cranial nerve, cranial nerve VII, or simply CN VII, is a cranial nerve that emerges from the pons of the brainstem, controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue. The nerve typically travels from the pons through the facial canal in the temporal bone and exits the skull at the stylomastoid foramen. It arises from the brainstem from an area posterior to the cranial nerve VI and anterior to cranial nerve VIII.
Articles related to anatomy include:
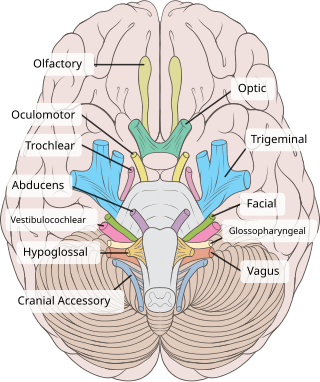
The oculomotor nerve, also known as the third cranial nerve, cranial nerve III, or simply CN III, is a cranial nerve that enters the orbit through the superior orbital fissure and innervates extraocular muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the intrinsic eye muscles that enable pupillary constriction and accommodation. The oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in control of eye movement.
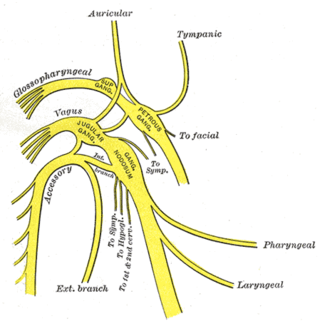
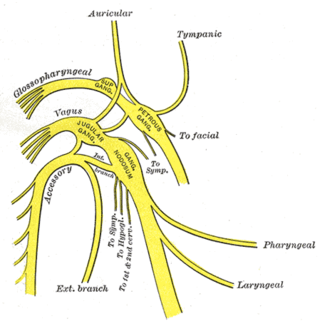
The glossopharyngeal nerve, also known as the ninth cranial nerve, cranial nerve IX, or simply CN IX, is a cranial nerve that exits the brainstem from the sides of the upper medulla, just anterior to the vagus nerve. Being a mixed nerve (sensorimotor), it carries afferent sensory and efferent motor information. The motor division of the glossopharyngeal nerve is derived from the basal plate of the embryonic medulla oblongata, whereas the sensory division originates from the cranial neural crest.
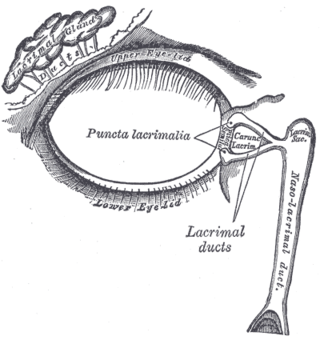
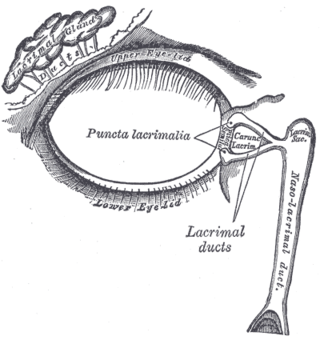
The lacrimal glands are paired exocrine glands, one for each eye, found in most terrestrial vertebrates and some marine mammals, that secrete the aqueous layer of the tear film. In humans, they are situated in the upper lateral region of each orbit, in the lacrimal fossa of the orbit formed by the frontal bone. Inflammation of the lacrimal glands is called dacryoadenitis. The lacrimal gland produces tears which are secreted by the lacrimal ducts, and flow over the ocular surface, and then into canals that connect to the lacrimal sac. From that sac, the tears drain through the lacrimal duct into the nose.

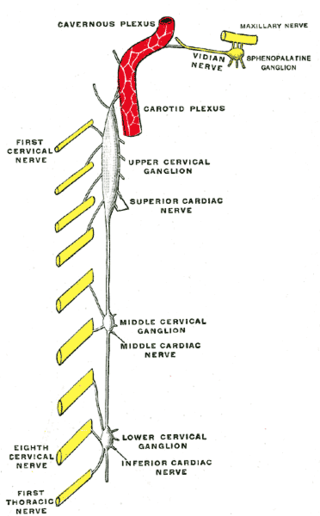
Horner's syndrome, also known as oculosympathetic paresis, is a combination of symptoms that arises when a group of nerves known as the sympathetic trunk is damaged. The signs and symptoms occur on the same side (ipsilateral) as it is a lesion of the sympathetic trunk. It is characterized by miosis, partial ptosis, apparent anhidrosis, with apparent enophthalmos.

The otic ganglion is a small parasympathetic ganglion located immediately below the foramen ovale in the infratemporal fossa and on the medial surface of the mandibular nerve. It is functionally associated with the glossopharyngeal nerve and innervates the parotid gland for salivation.

The pterygopalatine ganglion is a parasympathetic ganglion in the pterygopalatine fossa. It is one of four parasympathetic ganglia of the head and neck,.

The ciliary ganglion is a bundle of nerves, parasympathetic ganglion located just behind the eye in the posterior orbit. It is 1–2 mm in diameter and in humans contains approximately 2,500 neurons. The ganglion contains postganglionic parasympathetic neurons. These neurons supply the pupillary sphincter muscle, which constricts the pupil, and the ciliary muscle which contracts to make the lens more convex. Both of these muscles are involuntary since they are controlled by the parasympathetic division of the autonomic nervous system.
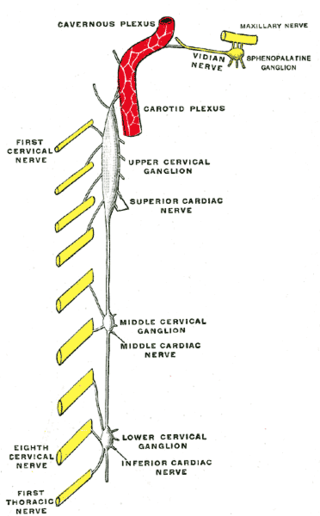
The superior cervical ganglion (SCG) is the upper-most and largest of the cervical sympathetic ganglia of the sympathetic trunk. It probably formed by the union of four sympathetic ganglia of the cervical spinal nerves C1–C4. It is the only ganglion of the sympathetic nervous system that innervates the head and neck. The SCG innervates numerous structures of the head and neck.

The long ciliary nerves are 2-3 nerves that arise from the nasociliary nerve (itself a branch of the ophthalmic branch (CN V1) of the trigeminal nerve (CN V)). They enter the eyeball to provide sensory innervation to parts of the eye, and sympathetic visceral motor innervation to the dilator pupillae muscle.

The submandibular ganglion is part of the human autonomic nervous system. It is one of four parasympathetic ganglia of the head and neck..

Parasympathetic ganglia are the autonomic ganglia of the parasympathetic nervous system. Most are small terminal ganglia or intramural ganglia, so named because they lie near or within (respectively) the organs they innervate. The exceptions are the four paired parasympathetic ganglia of the head and neck.

The short ciliary nerves are nerves of the orbit around the eye. They are branches of the ciliary ganglion. They supply parasympathetic and sympathetic nerve fibers to the ciliary muscle, iris, and cornea. Damage to the short ciliary nerve may result in loss of the pupillary light reflex, or mydriasis.

The lateral grey column is one of the three grey columns of the spinal cord ; the others being the anterior and posterior grey columns. The lateral grey column is primarily involved with activity in the sympathetic division of the autonomic motor system. It projects to the side as a triangular field in the thoracic and upper lumbar regions of the postero-lateral part of the anterior grey column.

The ciliospinal center is a cluster of pre-ganglionic sympathetic neuron cell bodies located in the intermediolateral cell column of the spinal cord at the (C8) T1-T2 spinal levels.

The following diagram is provided as an overview of and topical guide to the human nervous system: