The parasympathetic nervous system (PSNS) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

Mydriasis is the dilation of the pupil, usually having a non-physiological cause, or sometimes a physiological pupillary response. Non-physiological causes of mydriasis include disease, trauma, or the use of certain types of drug. It may also be of unknown cause.
Articles related to anatomy include:
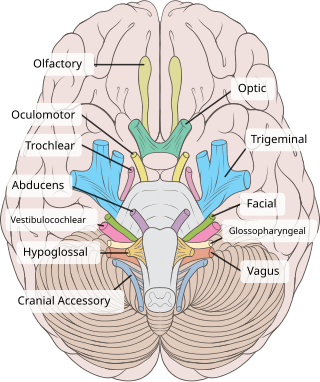
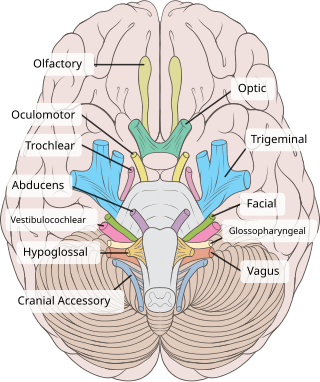
The oculomotor nerve, also known as the third cranial nerve, cranial nerve III, or simply CN III, is a cranial nerve that enters the orbit through the superior orbital fissure and innervates extraocular muscles that enable most movements of the eye and that raise the eyelid. The nerve also contains fibers that innervate the intrinsic eye muscles that enable pupillary constriction and accommodation. The oculomotor nerve is derived from the basal plate of the embryonic midbrain. Cranial nerves IV and VI also participate in control of eye movement.

The pupillary light reflex (PLR) or photopupillary reflex is a reflex that controls the diameter of the pupil, in response to the intensity (luminance) of light that falls on the retinal ganglion cells of the retina in the back of the eye, thereby assisting in adaptation of vision to various levels of lightness/darkness. A greater intensity of light causes the pupil to constrict, whereas a lower intensity of light causes the pupil to dilate. Thus, the pupillary light reflex regulates the intensity of light entering the eye. Light shone into one eye will cause both pupils to constrict.

The ciliary muscle is an intrinsic muscle of the eye formed as a ring of smooth muscle in the eye's middle layer, uvea. It controls accommodation for viewing objects at varying distances and regulates the flow of aqueous humor into Schlemm's canal. It also changes the shape of the lens within the eye but not the size of the pupil which is carried out by the sphincter pupillae muscle and dilator pupillae.

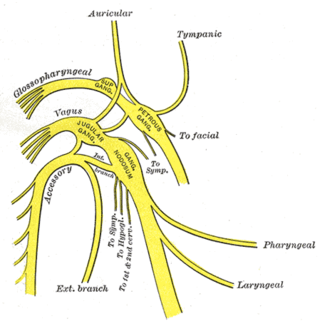
The otic ganglion is a small parasympathetic ganglion located immediately below the foramen ovale in the infratemporal fossa and on the medial surface of the mandibular nerve. It is functionally associated with the glossopharyngeal nerve and innervates the parotid gland for salivation.

The pterygopalatine ganglion is a parasympathetic ganglion in the pterygopalatine fossa. It is one of four parasympathetic ganglia of the head and neck,.

The ciliary ganglion is a parasympathetic ganglion located just behind the eye in the posterior orbit. It is 1–2 mm in diameter and in humans contains approximately 2,500 neurons. The ganglion contains postganglionic parasympathetic neurons. These neurons supply the pupillary sphincter muscle, which constricts the pupil, and the ciliary muscle which contracts to make the lens more convex. Both of these muscles are involuntary since they are controlled by the parasympathetic division of the autonomic nervous system.

The iris dilator muscle, is a smooth muscle of the eye, running radially in the iris and therefore fit as a dilator. The pupillary dilator consists of a spokelike arrangement of modified contractile cells called myoepithelial cells. These cells are stimulated by the sympathetic nervous system. When stimulated, the cells contract, widening the pupil and allowing more light to enter the eye.

The iris sphincter muscle is a muscle in the part of the eye called the iris. It encircles the pupil of the iris, appropriate to its function as a constrictor of the pupil.
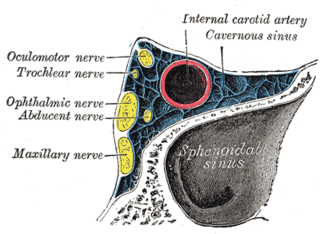
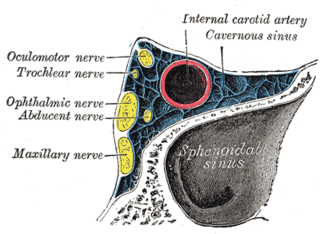
The ophthalmic nerve (CN V1) is a sensory nerve of the head. It is one of three divisions of the trigeminal nerve (CN V), a cranial nerve. It has three major branches which provide sensory innervation to the eye, and the skin of the upper face and anterior scalp, as well as other structures of the head.

The nasociliary nerve is a branch of the ophthalmic nerve (CN V1) (which is in turn a branch of the trigeminal nerve (CN V)). It is intermediate in size between the other two branches of the ophthalmic nerve, the frontal nerve and lacrimal nerve.

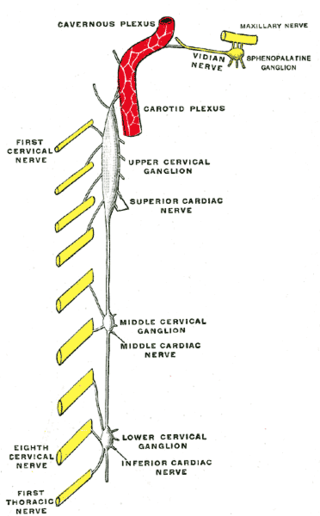
The internal carotid plexus is a nerve plexus situated upon the lateral side of the internal carotid artery. It is composed of post-ganglionic sympathetic fibres which have synapsed at the superior cervical ganglion. The plexus gives rise to the deep petrosal nerve.
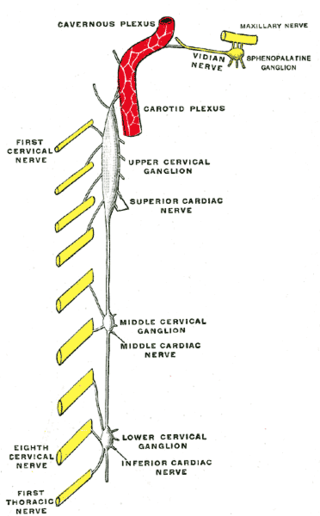
The superior cervical ganglion (SCG) is the upper-most and largest of the cervical sympathetic ganglia of the sympathetic trunk. It probably formed by the union of four sympathetic ganglia of the cervical spinal nerves C1–C4. It is the only ganglion of the sympathetic nervous system that innervates the head and neck. The SCG innervates numerous structures of the head and neck.

The long ciliary nerves are 2-3 nerves that arise from the nasociliary nerve (itself a branch of the ophthalmic branch (CN V1) of the trigeminal nerve (CN V)). They enter the eyeball to provide sensory innervation to parts of the eye, and sympathetic visceral motor innervation to the dilator pupillae muscle.
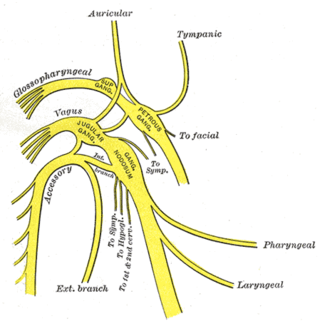
The tympanic nerve is a branch of the glossopharyngeal nerve found near the ear. It gives sensation to the middle ear, the Eustachian tube, the parotid gland, and mastoid air cells. It gives parasympathetic to supply to the parotid gland via the otic ganglion and the auriculotemporal nerve.
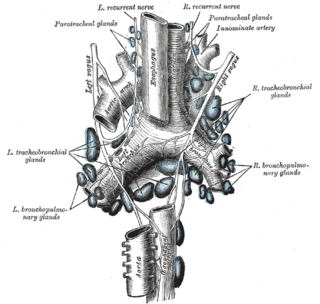
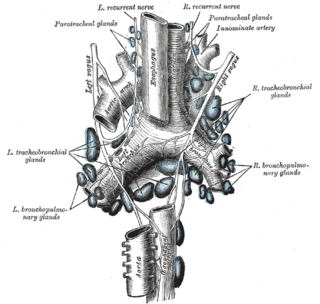
The esophageal plexus is formed by nerve fibers from two sources, branches of the vagus nerve, and visceral branches of the sympathetic trunk. The esophageal plexus and the cardiac plexus contain the same types of fibers and are both considered thoracic autonomic plexus.

The following diagram is provided as an overview of and topical guide to the human nervous system:

The ciliary ganglion is a parasympathetic ganglion located just behind the eye in the posterior orbit. Three types of axons enter the ciliary ganglion but only the preganglionic parasympathetic axons synapse there. The entering axons are arranged into three roots of the ciliary ganglion, which join enter the posterior surface of the ganglion.