The lungs are the primary organs of the respiratory system in humans and most other animals, including some snails and a small number of fish. In mammals and most other vertebrates, two lungs are located near the backbone on either side of the heart. Their function in the respiratory system is to extract oxygen from the air and transfer it into the bloodstream, and to release carbon dioxide from the bloodstream into the atmosphere, in a process of gas exchange. The pleurae, which are thin, smooth, and moist, serve to reduce friction between the lungs and chest wall during breathing, allowing for easy and effortless movements of the lungs.
Diffusing capacity of the lung (DL) measures the transfer of gas from air in the lung, to the red blood cells in lung blood vessels. It is part of a comprehensive series of pulmonary function tests to determine the overall ability of the lung to transport gas into and out of the blood. DL, especially DLCO, is reduced in certain diseases of the lung and heart. DLCO measurement has been standardized according to a position paper by a task force of the European Respiratory and American Thoracic Societies.

Lung volumes and lung capacities refer to the volume of air in the lungs at different phases of the respiratory cycle.

A spirometer is an apparatus for measuring the volume of air inspired and expired by the lungs. A spirometer measures ventilation, the movement of air into and out of the lungs. The spirogram will identify two different types of abnormal ventilation patterns, obstructive and restrictive. There are various types of spirometers that use a number of different methods for measurement.

Spirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.

A plethysmograph is an instrument for measuring changes in volume within an organ or whole body. The word is derived from the Greek "plethysmos", and "graphein".
Optoelectronic plethysmography is a method to evaluate ventilation through an external measurement of the chest wall surface motion.
DLCO or TLCO is the extent to which oxygen passes from the air sacs of the lungs into the blood. Commonly, it refers to the test used to determine this parameter. It was introduced in 1909.
Lung compliance, or pulmonary compliance, is a measure of the lung's ability to stretch and expand. In clinical practice it is separated into two different measurements, static compliance and dynamic compliance. Static lung compliance is the change in volume for any given applied pressure. Dynamic lung compliance is the compliance of the lung at any given time during actual movement of air.
The closing capacity (CC) is the volume in the lungs at which its smallest airways, the respiratory bronchioles, collapse. It is defined mathematically as the sum of the closing volume and the residual volume. The alveoli lack supporting cartilage and so depend on other factors to keep them open. The closing capacity is less than the Functional Residual Capacity, the amount of gas that normally remains in the lungs during respiration. This means that there is normally enough air within the lungs to keep these airways open throughout both inhalation and exhalation. As the lungs age, there is a gradual increase in the closing capacity. This also occurs with certain disease processes, such as asthma, chronic obstructive pulmonary disease, and pulmonary edema. Any process that increases the CC by increasing the closing volume (CV) can increase an individual's risk of hypoxemia, as the small airways may collapse during exhalation, leading to air trapping and atelectasis.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include; asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.
Restrictive lung diseases are a category of extrapulmonary, pleural, or parenchymal respiratory diseases that restrict lung expansion, resulting in a decreased lung volume, an increased work of breathing, and inadequate ventilation and/or oxygenation. Pulmonary function test demonstrates a decrease in the forced vital capacity.

Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a pulmonary function technician, respiratory therapist, respiratory physiologist, physiotherapist, pulmonologist, or general practitioner.
Nitrogen washout is a test for measuring anatomic dead space in the lung during a respiratory cycle, as well as some parameters related to the closure of airways.
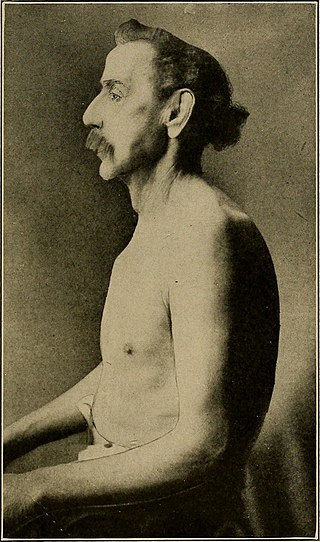
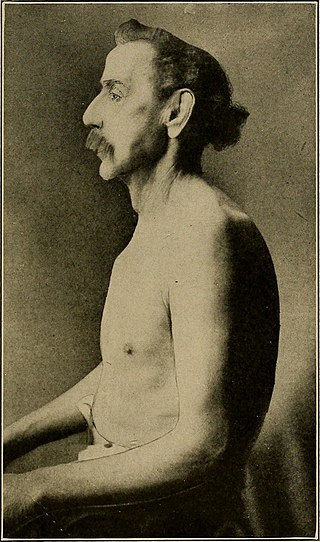
Barrel chest generally refers to a broad, deep chest found on a patient. A barrel chested person will usually have a naturally large ribcage, very round torso, large lung capacity, and can potentially have great upper body strength. It can sometimes be found alongside acromegaly. Barrel chest, as a medical condition, is most commonly related to osteoarthritis as individuals age. Arthritis can stiffen the chest causing the ribs to become fixed in their most expanded position, giving the appearance of a barrel chest.

Breathing is the process of moving air into and from the lungs to facilitate gas exchange with the internal environment, mostly to flush out carbon dioxide and bring in oxygen.
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of the management and health maintenance of people with chronic respiratory disease who remain symptomatic or continue to have decreased function despite standard medical treatment. It is a broad therapeutic concept. It is defined by the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. In general, pulmonary rehabilitation refers to a series of services that are administered to patients of respiratory disease and their families, typically to attempt to improve the quality of life for the patient. Pulmonary rehabilitation may be carried out in a variety of settings, depending on the patient's needs, and may or may not include pharmacologic intervention.

Emphysema is any air-filled enlargement in the body's tissues. Most commonly emphysema refers to the enlargement of air spaces (alveoli) in the lungs, and is also known as pulmonary emphysema.
A respiratory pressure meter measures the maximum inspiratory and expiratory pressures that a patient can generate at either the mouth (MIP and MEP) or inspiratory pressure a patient can generate through their nose via a sniff manoeuvre (SNIP). These measurements require patient cooperation and are known as volitional tests of respiratory muscle strength. Handheld devices displaying the measurement achieved in cmH2O and the pressure trace created, allow quick patient testing away from the traditional pulmonary laboratory and are useful for ward based, out patient, and preoperative assessment as well as for use by pulmonologists and physiotherapists.
Collateral ventilation is a back-up system of alveolar ventilation that can bypass the normal route of airflow when airways are restricted or obstructed. The pathways involved include those between adjacent alveoli, between bronchioles and alveoli, and those between bronchioles . Collateral ventilation also serves to modulate imbalances in ventilation and perfusion a feature of many diseases. The pathways are altered in lung diseases particularly asthma, and emphysema. A similar functional pattern of collateralisation is seen in the circulatory system of the heart.