Heroin, also known as diacetylmorphine and diamorphine among other names, is a morphinan opioid substance synthesized from the dried latex of the Papaver somniferum plant; it is mainly used as a recreational drug for its euphoric effects. Medical-grade diamorphine is used as a pure hydrochloride salt. Various white and brown powders sold illegally around the world as heroin are routinely diluted with cutting agents. Black tar heroin is a variable admixture of morphine derivatives—predominantly 6-MAM (6-monoacetylmorphine), which is the result of crude acetylation during clandestine production of street heroin. Heroin is used medically in several countries to relieve pain, such as during childbirth or a heart attack, as well as in opioid replacement therapy.

Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for chronic pain and also for opioid use disorder. It is used to treat chronic pain, and it is also used to treat addiction to heroin or other opioids. Prescribed for daily use, the medicine relieves cravings and removes withdrawal symptoms. Withdrawal management using methadone can be accomplished in less than a month, or it may be done gradually over a longer period of time, or simply maintained for the rest of the patient's life. While a single dose has a rapid effect, maximum effect can take up to five days of use. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.

Harm reduction, or harm minimization, refers to a range of intentional practices and public health policies designed to lessen the negative social and/or physical consequences associated with various human behaviors, both legal and illegal. Harm reduction is used to decrease negative consequences of recreational drug use and sexual activity without requiring abstinence, recognizing that those unable or unwilling to stop can still make positive change to protect themselves and others.

Fentanyl is a potent synthetic piperidine opioid primarily used as an analgesic. It is 50 times more potent than heroin and 100 times more potent than morphine; its primary clinical utility is in pain management for cancer patients and those recovering from painful surgeries. Fentanyl is also used as a sedative. Depending on the method of delivery, fentanyl can be very fast acting and ingesting a relatively small quantity can cause overdose. Fentanyl works by activating μ-opioid receptors. Fentanyl is sold under the brand names Actiq, Duragesic and Sublimaze, among others.

A drug overdose is the ingestion or application of a drug or other substance in quantities much greater than are recommended. Typically it is used for cases when a risk to health will potentially result. An overdose may result in a toxic state or death.

Supervised injection sites (SIS) or drug consumption rooms (DCRs) are a health and social response to drug-related problems. They are fixed or mobile spaces where people who use drugs are provided with sterile drug use equipment and can use illicit drugs under the supervision of trained staff. They are usually located in areas where there is an open drug scene and where injecting in public places is common. The primary target group for DCR services are people who engage in risky drug use.

Opioid use disorder (OUD) is a substance use disorder characterized by cravings for opioids, continued use despite physical and/or psychological deterioration, increased tolerance with use, and withdrawal symptoms after discontinuing opioids. Opioid withdrawal symptoms include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are important components of opioid use disorder.

Drug injection is a method of introducing a drug into the bloodstream via a hollow hypodermic needle, which is pierced through the skin into the body. Intravenous therapy, a form of drug injection, is universally practiced in modernized medical care. As of 2004, there were 13.2 million people worldwide who self-administered injection drugs outside of medical supervision, of which 22% are from developed countries.
Illicit drug use in Australia is the recreational use of prohibited drugs in Australia. Illicit drugs include illegal drugs, pharmaceutical drugs when used for non-medical purposes, and other substances used inappropriately. According to government and community organisations, the use and abuse, and the illegality, of illicit drugs is a social, health and legal issue that creates an annual illegal market estimated to be worth A$6.7 billion. Estimates made in 2022 place the figure at A$11.3 billion per year.
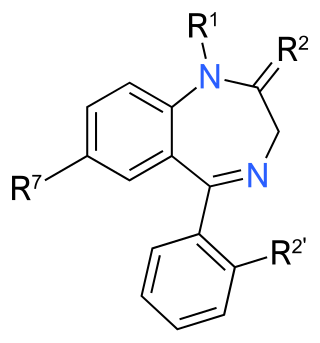
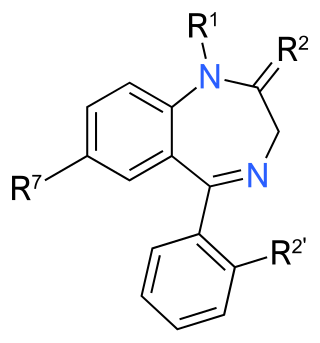
Benzodiazepine use disorder (BUD), also called misuse or abuse, is the use of benzodiazepines without a prescription and/or for recreational purposes, which poses risks of dependence, withdrawal and other long-term effects. Benzodiazepines are one of the more common prescription drugs used recreationally. When used recreationally benzodiazepines are usually administered orally but sometimes they are taken intranasally or intravenously. Recreational use produces effects similar to alcohol intoxication.
Heroin-assisted treatment (HAT), or diamorphine-assisted treatment, refers to a type of Medication-Assisted Treatment (MAT) where semi-synthetic heroin is prescribed to opiate addicts who do not benefit from, or cannot tolerate, treatment with one of the established drugs used in opiate replacement therapy such as methadone or buprenorphine. For this group of patients, heroin-assisted treatment has proven superior in improving their social and health situation. Heroin-assisted treatment is fully a part of the national health system in Switzerland, Germany, the Netherlands, Canada, and Denmark. Additional trials are being carried out in the United Kingdom, Norway, and Belgium.

Substance use disorder (SUD) is the persistent use of drugs despite the substantial harm and adverse consequences to one's own self and others, as a result of their use. In perspective, the effects of the wrong use of substances that are capable of causing harm to the user or others, have been extensively described in different studies using a variety of terms such as substance use problems, problematic drugs or alcohol use, and substance use disorder. The National Institute of Mental Health (NIMH) states that "Substance use disorder (SUD) is a treatable mental disorder that affects a person's brain and behavior, leading to their inability to control their use of substances like legal or illegal drugs, alcohol, or medications. Symptoms can be moderate to severe, with addiction being the most severe form of SUD". Substance use disorders (SUD) are considered to be a serious mental illness that fluctuates with the age that symptoms first start appearing in an individual, the time during which it exists and the type of substance that is used. It is not uncommon for those who have SUD to also have other mental health disorders. Substance use disorders are characterized by an array of mental/emotional, physical, and behavioral problems such as chronic guilt; an inability to reduce or stop consuming the substance(s) despite repeated attempts; operating vehicles while intoxicated; and physiological withdrawal symptoms. Drug classes that are commonly involved in SUD include: alcohol (alcoholism); cannabis; opioids; stimulants such as nicotine, cocaine and amphetamines; benzodiazepines; barbiturates; and other substances.

Acetylfentanyl is an opioid analgesic drug that is an analog of fentanyl. Studies have estimated acetylfentanyl to be 15 times more potent than morphine, which would mean that despite being somewhat weaker than fentanyl, it is nevertheless still several times stronger than pure heroin. It has never been licensed for medical use and instead has only been sold on the illicit drug market. Acetylfentanyl was discovered at the same time as fentanyl itself and had only rarely been encountered on the illicit market in the late 1980s. However, in 2013, Canadian police seized 3 kilograms of acetylfentanyl. As a μ-opioid receptor agonist, acetylfentanyl may serve as a direct substitute for oxycodone, heroin or other opioids. Common side effects of fentanyl analogs are similar to those of fentanyl itself, which include itching, nausea and potentially fatal respiratory depression. Fentanyl analogs have killed hundreds of people throughout Europe and the former Soviet republics since the most recent resurgence in use began in Estonia in the early 2000s, and novel derivatives continue to appear.

Under Australia's law, methamphetamine is a Schedule 8 drug, available for medical use but restricted in manufacture, supply, and possession. The drug is sought after to give oneself a ‘high’ or a ‘rush’ in their body. Users of this drug often feel senses of exhilaration and arousal as the brain is flooded with monoamines. Methamphetamine has many names not only in Australia, but also around the world. These include chalk, crypto, gear, getgo, tweak, and cristy, although the two most common ones in Australia today are ice and shard. Speed refers to the powder form of the drug, while ice refers to the highly purified, crystalline form. The powder form is often diluted with adulterants including glucose and sucrose.

There is an ongoing opioid epidemic in the United States, originating out of both medical prescriptions and illegal sources. The epidemic began in the United States in the late 1990s, according to the Centers for Disease Control and Prevention (CDC), when opioids were increasingly prescribed for pain management, resulting in a rise in overall opioid use throughout subsequent years.
Discrimination against drug addicts is a form of discrimination against people who suffer from a drug addiction.
A take-home naloxone program is a governmental program that provides naloxone drug kits to those that are at risk of an opioid overdose. Naloxone is a medication that was created to reverse opioid overdoses. As an opioid antagonist, it binds to the μ-opioid receptors blocking the opioid's effects. Naloxone quickly restores normal respiration. The ongoing opioid epidemic has caused many public health authorities to expand access to naloxone.

The Uniting Medically Supervised Injecting Centre Kings Cross is a state government-supported facility in Kings Cross, New South Wales that provides safe injecting rooms, sterile equipment and medical supervision for individuals who wish to administer an illicit drug intravenously.
Opioid agonist therapy (OAT) is a treatment in which prescribed opioid agonists are given to patients who live with Opioid use disorder (OUD). In the case of methadone maintenance treatment (MMT), methadone is used to treat dependence on heroin or other opioids, and is administered on an ongoing basis.
Harm reduction consists of a series of strategies aimed at reducing the negative impacts of drug use on users. It has been described as an alternative to the U.S.'s moral model and disease model of drug use and addiction. While the moral model treats drug use as a morally wrong action and the disease model treats it as a biological or genetic disease needing medical intervention, harm reduction takes a public health approach with a basis in pragmatism. Harm reduction provides an alternative to complete abstinence as a method for preventing and mitigating the negative consequences of drug use and addiction.