Acne, also known as acne vulgaris, is a long-term skin condition that occurs when dead skin cells and oil from the skin clog hair follicles. Typical features of the condition include blackheads or whiteheads, pimples, oily skin, and possible scarring. It primarily affects skin with a relatively high number of oil glands, including the face, upper part of the chest, and back. The resulting appearance can lead to lack of confidence, anxiety, reduced self-esteem, and, in extreme cases, depression or thoughts of suicide.
Intense pulsed light (IPL) is a technology used by cosmetic and medical practitioners to perform various skin treatments for aesthetic and therapeutic purposes, including hair removal, photorejuvenation as well as to alleviate dermatologic diseases such as acne. IPL is increasingly used in optometry and ophthalmology as well, to treat evaporative dry eye disease due to meibomian gland dysfunction.

A sebaceous gland or oil gland is a microscopic exocrine gland in the skin that opens into a hair follicle to secrete an oily or waxy matter, called sebum, which lubricates the hair and skin of mammals. In humans, sebaceous glands occur in the greatest number on the face and scalp, but also on all parts of the skin except the palms of the hands and soles of the feet. In the eyelids, meibomian glands, also called tarsal glands, are a type of sebaceous gland that secrete a special type of sebum into tears. Surrounding the female nipple, areolar glands are specialized sebaceous glands for lubricating the nipple. Fordyce spots are benign, visible, sebaceous glands found usually on the lips, gums and inner cheeks, and genitals.

Cutibacterium acnes is the relatively slow-growing, typically aerotolerant anaerobic, gram-positive bacterium (rod) linked to the skin condition of acne; it can also cause chronic blepharitis and endophthalmitis, the latter particularly following intraocular surgery. Its genome has been sequenced and a study has shown several genes can generate enzymes for degrading skin and proteins that may be immunogenic.

Rosacea is a long-term skin condition that typically affects the face. It results in redness, pimples, swelling, and small and superficial dilated blood vessels. Often, the nose, cheeks, forehead, and chin are most involved. A red, enlarged nose may occur in severe disease, a condition known as rhinophyma.

A boil, also called a furuncle, is a deep folliculitis, which is an infection of the hair follicle. It is most commonly caused by infection by the bacterium Staphylococcus aureus, resulting in a painful swollen area on the skin caused by an accumulation of pus and dead tissue. Boils are therefore basically pus-filled nodules. Individual boils clustered together are called carbuncles. Most human infections are caused by coagulase-positive S. aureus strains, notable for the bacteria's ability to produce coagulase, an enzyme that can clot blood. Almost any organ system can be infected by S. aureus.

Hyperpigmentation is the darkening of an area of skin or nails caused by increased melanin.
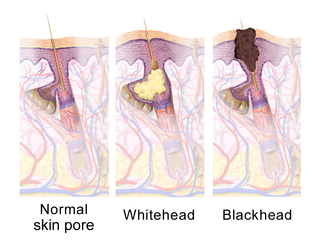
A comedo is a clogged hair follicle (pore) in the skin. Keratin combines with oil to block the follicle. A comedo can be open (blackhead) or closed by skin (whitehead) and occur with or without acne. The word "comedo" comes from the Latin comedere, meaning "to eat up", and was historically used to describe parasitic worms; in modern medical terminology, it is used to suggest the worm-like appearance of the expressed material.

Pyoderma gangrenosum is a rare, inflammatory skin disease where painful pustules or nodules become ulcers that progressively grow. Pyoderma gangrenosum is not infectious.
A sitting disability is a condition in which a person has difficulties sitting or is unable to do so at all; usually due to pain. This can affect people who face little or no chronic problems with standing, as well as those who do, such as mobility aid users.
Hidradenitis is any disease in which the histologic abnormality is primarily an inflammatory infiltrate around the eccrine glands. This group includes neutrophilic eccrine hidradenitis and recurrent palmoplantar hidradenitis.

Nadifloxacin is a topical fluoroquinolone antibiotic for the treatment of acne vulgaris. It is also used to treat bacterial skin infections.

Neonatal acne, also known as acne neonatorum, is a type of acne that develops in newborns, typically before 6 weeks of life. It presents with open and closed comedones on the cheeks, chin and forehead.
Acne necrotica presents with a primary lesion that is a pruritic or painful erythematous follicular-based papule that develops central necrosis and crusting and heals with a varioliform scar.
Neutrophilic eccrine hidradenitis (NEH) usually is a cutaneous complication of chemotherapy, but it can also occur for other reasons. It consists of fever and non specific skin lesions. It is rare, and self-limited.
Recurrent palmoplantar hidradenitis, also known as idiopathic palmoplantar hidradenitis, idiopathic plantar hidradenitis, painful plantar erythema, palmoplantar eccrine hidradenitis, and plantar panniculitis, is primarily a disorder of healthy children and young adults, characterized by lesions that are primarily painful, subcutaneous nodules on the plantar surface, resembling erythema nodosum.

A pimple or zit is a kind of comedo that results from excess sebum and dead skin cells getting trapped in the pores of the skin. In its aggravated state, it may evolve into a pustule or papule. Pimples can be treated by acne medications, antibiotics, and anti-inflammatories prescribed by a physician, or various over the counter remedies purchased at a pharmacy.
Infantile acne is a form of acne that begins in very young children. Typical symptoms include inflammatory and noninflammatory lesions, papules and pustules most commonly present on the face. No cause of infantile acne has been established but it may be caused by increased sebaceous gland secretions due to elevated androgens, genetics and the fetal adrenal gland causing increased sebum production. Infantile acne can resolve by itself by age 1 or 2. However, treatment options include topical benzyl peroxide, topical retinoids and topical antibiotics in most cases.
Idiopathic pure sudomotor failure (IPSF) is the most common cause of a rare disorder known as acquired idiopathic generalized anhidrosis (AIGA), a clinical syndrome characterized by generalized decrease or absence of sweating without other autonomic and somatic nervous dysfunctions and without persistent organic cutaneous lesions.

Clascoterone, sold under the brand name Winlevi, is an antiandrogen medication which is used topically in the treatment of acne. It is also under development in a higher concentration for the treatment of androgen-dependent scalp hair loss, under the brand name Breezula. The medication is used as a cream by application to the skin, for instance the face and scalp.





![Micrograph of hidradenitis suppurativa: Sinus tracts [(A), arrow], active inflammation, and rupture [(B), asterisks] of the follicular epithelium with "floating" hair fragments (B), arrowSubsequently, a secondary inflammatory response is induced with influx of numerous neutrophils [(C), arrows] and granulomatous foreign body reaction with giant cells [(C), asterisks]. Micrograph of hidradenitis suppurativa.jpg](http://upload.wikimedia.org/wikipedia/commons/thumb/3/3d/Micrograph_of_hidradenitis_suppurativa.jpg/220px-Micrograph_of_hidradenitis_suppurativa.jpg)