Hidradenitis suppurativa (HS), also known as acne inversa, is a long term skin disease characterized by the occurrence of inflamed and swollen lumps. These are typically painful and break open, releasing fluid or pus. The areas most commonly affected are the underarms, under the breasts, and groin. Scar tissue remains after healing. Self-consciousness or depression may result.
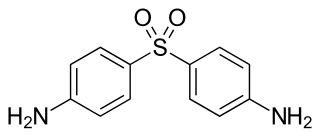
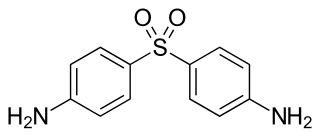
Dapsone, also known as diaminodiphenyl sulfone (DDS), is an antibiotic commonly used in combination with rifampicin and clofazimine for the treatment of leprosy. It is a second-line medication for the treatment and prevention of pneumocystis pneumonia and for the prevention of toxoplasmosis in those who have poor immune function. Additionally, it has been used for acne, dermatitis herpetiformis, and various other skin conditions. Dapsone is available both topically and by mouth.

Lichen planus (LP) is a chronic inflammatory and immune mediated disease that affects the skin, nails, hair, and mucous membranes. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

Dermatofibrosarcoma protuberans (DFSP) is a rare tumor of the dermis layer of the skin, and is classified as a sarcoma. There is only about one case per million per year. DFSP is a fibrosarcoma, more precisely a cutaneous soft tissue sarcoma. In many respects, the disease behaves as a benign tumor, but in 2–5% of cases it can metastasize, so it should be considered to have malignant potential. It occurs most often in adults in their thirties; it has been described congenitally, in children, and the elderly. It accounts for approximately 2–6% of soft tissue sarcoma cancers.

Pemphigus is a rare group of blistering autoimmune diseases that affect the skin and mucous membranes. The name is derived from the Greek root "pemphix," meaning "pustule."

Livedo reticularis is a common skin finding consisting of a mottled reticulated vascular pattern that appears as a lace-like purplish discoloration of the skin. The discoloration is caused by swelling of the venules owing to obstruction of capillaries by small blood clots. The blood clots in the small blood vessels can be a secondary effect of a condition that increases a person's risk of forming blood clots, including a wide array of pathological and nonpathological conditions. Examples include hyperlipidemia, microvascular hematological or anemia states, nutritional deficiencies, hyper- and autoimmune diseases, and drugs/toxins.

Sweet's syndrome (SS), or acute febrile neutrophilic dermatosis is a skin disease characterized by the sudden onset of fever, an elevated white blood cell count, and tender, red, well-demarcated papules and plaques that show dense infiltrates by neutrophil granulocytes on histologic examination.

Erythema anulare centrifugum (EAC), is a descriptive term for a class of skin lesion presenting redness (erythema) in a ring form (anulare) that spreads from a center (centrifugum). It was first described by Darier in 1916. Many different terms have been used to classify these types of lesions and it is still controversial on what exactly defines EAC. Some of the types include annular erythema, erythema perstans, erythema gyratum perstans, erythema gyratum repens, darier erythema and erythema figuratum perstans.

Grover's disease (GD) is a polymorphic, pruritic, papulovesicular dermatosis characterized histologically by acantholysis with or without dyskeratosis. Once confirmed, most cases of Grover's disease last six to twelve months, which is why it was originally called "transient". However it may last much longer. Nevertheless, it is not to be confused with relapsing linear acantholytic dermatosis.
Hidradenitis is any disease in which the histologic abnormality is primarily an inflammatory infiltrate around the eccrine glands. This group includes neutrophilic eccrine hidradenitis and recurrent palmoplantar hidradenitis.

Chemotherapy-induced acral erythema is reddening, swelling, numbness and desquamation on palms of the hands and soles of the feet that can occur after chemotherapy in patients with cancer. Hand-foot syndrome is also rarely seen in sickle-cell disease. These skin changes usually are well demarcated. Acral erythema typically disappears within a few weeks after discontinuation of the offending drug.
Florid cutaneous papillomatosis (FCP), is an obligate paraneoplastic syndrome.
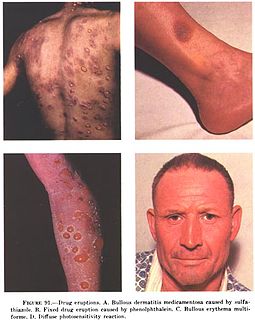
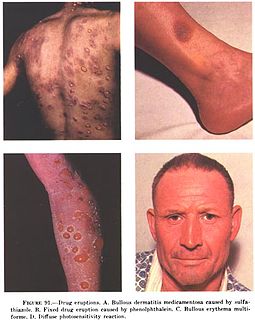
In medicine, a drug eruption is an adverse drug reaction of the skin. Most drug-induced cutaneous reactions are mild and disappear when the offending drug is withdrawn. These are called "simple" drug eruptions. However, more serious drug eruptions may be associated with organ injury such as liver or kidney damage and are categorized as "complex". Drugs can also cause hair and nail changes, affect the mucous membranes, or cause itching without outward skin changes.

Cutaneous small-vessel vasculitis (CSVV), also known as hypersensitivity vasculitis, cutaneous leukocytoclastic vasculitis, hypersensitivity angiitis, cutaneous leukocytoclastic angiitis, cutaneous necrotizing vasculitis and cutaneous necrotizing venulitis, is inflammation of small blood vessels, characterized by palpable purpura. It is the most common vasculitis seen in clinical practice.
Papillary eccrine adenoma is a cutaneous condition characterized by an uncommon benign sweat gland neoplasm that presents as a dermal nodule located primarily on the extremities of black patients.

Nevus depigmentosus is a loss of pigment in the skin which can be easily differentiated from vitiligo. Although age factor has not much involvement in the nevus depigmentosus but in about 19% of the cases these are noted at birth. Their size may however grow in proportion to growth of the body. The distribution is also fairly stable and are nonprogressive hypopigmented patches. The exact cause of nevus depigmentosus is still not clearly understood. A sporadic defect in the embryonic development has been suggested to be a causative factor. It has been described as "localised albinism", though this is incorrect.
Porokeratotic eccrine ostial and dermal duct nevus is a skin lesion that resembles a comedonal nevus, but it occurs on the palms and soles where pilosebaceous follicles are normally absent. It is probably transmitted by paradominant transmission.
Idiopathic pure sudomotor failure (IPSF) is the most common cause of a rare disorder known as acquired idiopathic generalized anhidrosis (AIGA), a clinical syndrome characterized by generalized decrease or absence of sweating without other autonomic and somatic nervous dysfunctions and without persistent organic cutaneous lesions.