The ovary is a gonad in the female reproductive system that produces ova. When an ovum is released, this travels through the fallopian tube into the uterus. There is an ovary found on the left and the right side of the body. The ovaries also secrete hormones that play a role in the menstrual cycle and fertility. The ovary progresses through many stages beginning in the prenatal period through menopause. It is also an endocrine gland because of the various hormones that it secretes.
Oophorectomy, historically also called ovariotomy, is the surgical removal of an ovary or ovaries. The surgery is also called ovariectomy, but this term is mostly used in reference to non-human animals, e.g. the surgical removal of ovaries from laboratory animals. Removal of the ovaries of females is the biological equivalent of castration of males; the term castration is only occasionally used in the medical literature to refer to oophorectomy of women. In veterinary medicine, the removal of ovaries and uterus is called ovariohysterectomy (spaying) and is a form of sterilization.

Breast cancer type 1 susceptibility protein is a protein that in humans is encoded by the BRCA1 gene. Orthologs are common in other vertebrate species, whereas invertebrate genomes may encode a more distantly related gene. BRCA1 is a human tumor suppressor gene and is responsible for repairing DNA.

Endometrial cancer is a cancer that arises from the endometrium. It is the result of the abnormal growth of cells that have the ability to invade or spread to other parts of the body. The first sign is most often vaginal bleeding not associated with a menstrual period. Other symptoms include pain with urination, pain during sexual intercourse, or pelvic pain. Endometrial cancer occurs most commonly after menopause.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

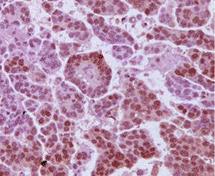
Ovarian clear-cell carcinoma, or clear-cell carcinoma of the ovary, also called ovarian clear-cell adenocarcinoma, is one of several subtypes of ovarian carcinoma – a subtype of epithelial ovarian cancer, in contrast to non-epithelial cancers. According to research, most ovarian cancers start at the epithelial layer which is the lining of the ovary. Within this epithelial group ovarian clear-cell carcinoma makes up 5–10%.

A serous tumour is a neoplasm that typically has papillary to solid formations of tumor cells with crowded nuclei, and which typically arises on the modified Müllerian-derived serous membranes that surround the ovaries in females. Such ovarian tumors are part of the surface epithelial-stromal tumour group of ovarian tumors. They are common neoplasms with a strong tendency to occur bilaterally, and they account for approximately a quarter of all ovarian tumors.

Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in this group are thought to be derived from the ovarian surface epithelium or from ectopic endometrial or fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This group of tumors accounts for 90% to 95% of all cases of ovarian cancer; however is mainly only found in postmenopausal women with the exception of the United States where 7% of cases occur in women under the age of 40. Serum CA-125 is often elevated but is only 50% accurate so it is not a useful tumor marker to assess the progress of treatment. 75% of women with epithelial ovarian cancer are found within the advanced-stages; however younger patients are more likely to have better prognoses than older patients.
In medicine, Meigs's syndrome, also Meigs syndrome or Demons–Meigs syndrome, is the triad of ascites, pleural effusion, and benign ovarian tumor. Meigs syndrome resolves after the resection of the tumor. Because the transdiaphragmatic lymphatic channels are larger in diameter on the right, the pleural effusion is classically on the right side. The causes of the ascites and pleural effusion are poorly understood. Atypical Meigs syndrome, characterized by a benign pelvic mass with right-sided pleural effusion but without ascites, can also occur. As in typical Meigs syndrome, pleural effusion resolves after removal of the pelvic mass.

Primary peritoneal cancer or carcinoma is also known as serous surface papillary carcinoma, primary peritoneal carcinoma, extra-ovarian serous carcinoma, primary serous papillary carcinoma, and psammomacarcinoma. It was historically classified under "carcinoma of unknown primary" (CUP). Primary peritoneal cancer is a cancer of the cells lining the peritoneum, or abdominal cavity.

Hereditary breast–ovarian cancer syndromes (HBOC) are cancer syndromes that produce higher than normal levels of breast cancer, ovarian cancer and additional cancers in genetically related families. It accounts for 90% of the hereditary cancers. The hereditary factors may be proven or suspected to cause the pattern of breast and ovarian cancer occurrences in the family. The name HBOC may be misleading because it implies that this genetic susceptibility to cancer is mainly in women. In reality, both sexes have the same rates of gene mutations and HBOC can predispose to other cancers including prostate cancer and pancreatic cancer. For this reason, the term "King syndrome" has recently come into use. The new name references Mary-Claire King who identified the genes BRCA1 and BRCA2.
Gynecologic cancer is a type of cancer that affects the female reproductive system, including ovarian cancer, uterine cancer, vaginal cancer, cervical cancer, and vulvar cancer.
Primary fallopian tube cancer (PFTC), often just tubal cancer, is a malignant neoplasm that originates from the fallopian tube.

A BRCA mutation is a mutation in either of the BRCA1 and BRCA2 genes, which are tumour suppressor genes. Hundreds of different types of mutations in these genes have been identified, some of which have been determined to be harmful, while others have no proven impact. Harmful mutations in these genes may produce a hereditary breast–ovarian cancer syndrome in affected persons. Only 5–10% of breast cancer cases in women are attributed to BRCA1 and BRCA2 mutations, but the impact on women with the gene mutation is more profound. Women with harmful mutations in either BRCA1 or BRCA2 have a risk of breast cancer that is about five times the normal risk, and a risk of ovarian cancer that is about ten to thirty times normal. The risk of breast and ovarian cancer is higher for women with a high-risk BRCA1 mutation than with a BRCA2 mutation. Having a high-risk mutation does not guarantee that the woman will develop any type of cancer, or imply that any cancer that appears was actually caused by the mutation, rather than some other factor.

Prophylactic salpingectomy is a preventative surgical technique performed on patients who are at higher risk of having ovarian cancer, such as individuals who may have pathogenic variants of the BRCA1 or BRCA2 gene. Originally salpingectomy was used in cases of ectopic pregnancies. As a preventative surgery however, it involves the removal of the fallopian tubes. By not removing the ovaries this procedure is advantageous to individuals who are still of child bearing age. It also reduces risks such as cardiovascular disease and osteoporosis which are associated with removal of the ovaries.
Professor James D Brenton is a clinician scientist and Senior Group Leader at the Cancer Research UK Cambridge Institute and Professor of Ovarian Cancer Medicine in the Department of Oncology, University of Cambridge. He is an Honorary Consultant in Medical Oncology at Addenbrooke's Hospital, Cambridge University Hospitals, Ovarian Cancer Domain Lead for the 100,000 Genomes Project by Genomics England, and co-founder and Clinical Advisor to Inivata Ltd, a clinical cancer genomics company.
Bradley J. Monk is an American gynecologic oncologist, academician and researcher. He is a Professor on the Clinical Scholar Track in the Department of Obstetrics and Gynecology at the University of Arizona College of Medicine in Phoenix, Arizona, as well as at the Creighton University School of Medicine in Omaha, Nebraska. He also serves as Director of the Division of Gynecologic Oncology at the St. Joseph's Hospital and Medical Center in Phoenix.

Breast and ovarian cancer does not necessarily imply that both cancers occur at the same time, but rather that getting one cancer would lead to the development of the other within a few years. Women with a history of breast cancer have a higher chance of developing ovarian cancer, vice versa.

The SEE-FIM protocol is a pathology dissection protocol for Sectioning and Extensively Examining the Fimbria (SEE-FIM). This protocol is intended to provide for the optimal microscopic examination of the distal fallopian tube (fimbria) to identify either cancerous or precancerous conditions in this organ.

Ovarian squamous cell carcinoma (oSCC) or squamous ovarian carcinoma (SOC) is a rare tumor that accounts for 1% of ovarian cancers. Included in the World Health Organization's classification of ovarian cancer, it mainly affects women above 45 years of age. Survival depends on how advanced the disease is and how different or similar the individual cancer cells are.