Dermatitis is a term used for different types of skin inflammation, typically characterized by itchiness, redness and a rash. In cases of short duration, there may be small blisters, while in long-term cases the skin may become thickened. The area of skin involved can vary from small to covering the entire body. Dermatitis is also called eczema but the same term is often used for the most common type of skin inflammation, atopic dermatitis.

Tinea cruris, also known as jock itch, is a common type of contagious, superficial fungal infection of the groin and buttocks region, which occurs predominantly but not exclusively in men and in hot-humid climates.

Irritant diaper dermatitis is a generic term applied to skin rash in the diaper area that are caused by various skin disorders and/or irritants.

Contact dermatitis is a type of acute or chronic inflammation of the skin caused by exposure to chemical or physical agents. Symptoms of contact dermatitis can include itchy or dry skin, a red rash, bumps, blisters, or swelling. These rashes are not contagious or life-threatening, but can be very uncomfortable.

Erythema multiforme (EM) is a skin condition that appears with red patches evolving into target lesions, typically on both hands.

A papule is a small, well-defined bump in the skin. It may have a rounded, pointed or flat top, and may have a dip. It can appear with a stalk, be thread-like or look warty. It can be soft or firm and its surface may be rough or smooth. Some have crusts or scales. A papule can be flesh colored, yellow, white, brown, red, blue or purplish. There may be just one or many, and they may occur irregularly in different parts of the body or appear in clusters. It does not contain fluid but may progress to a pustule or vesicle. A papule is smaller than a nodule; it can be as tiny as a pinhead and is typically less than 1 cm in width, according to some sources, and 0.5 cm according to others. When merged together, it appears as a plaque.

Dyshidrosis is a type of dermatitis, characterized by itchy vesicles of 1–2 mm in size, on the palms of the hands, sides of fingers, or bottoms of the feet. Outbreaks usually conclude within three to four weeks, but often recur. Repeated attacks may result in fissures and skin thickening. The cause of the condition is not known.

Urushiol-induced contact dermatitis is a type of allergic contact dermatitis caused by the oil urushiol found in various plants, most notably sumac family species of the genus Toxicodendron: poison ivy, poison oak, poison sumac, and the Chinese lacquer tree. The name is derived from the Japanese word for the sap of the Chinese lacquer tree, urushi. Other plants in the sumac family also contain urushiol, as do unrelated plants such as Ginkgo biloba.

Polymorphous light eruption (PLE) presents with itchy red small bumps on sun-exposed skin, particularly face, neck, forearms and legs. It generally appears 30 minutes to a few hours after sun exposure and may last between one and 14 days. The bumps may become small blisters or plaques and may appear bloody,often healing with minimal scarring.

Allergic contact dermatitis (ACD) is a form of contact dermatitis that is the manifestation of an allergic response caused by contact with a substance; the other type being irritant contact dermatitis (ICD).

Erythema migrans or erythema chronicum migrans is an expanding rash often seen in the early stage of Lyme disease, and can also be caused by southern tick-associated rash illness (STARI). It can appear anywhere from one day to one month after a tick bite. This rash does not represent an allergic reaction to the bite, but rather an actual skin infection of one of the Lyme bacteria species from the genus Borrelia. The rash's name comes from Neo-Latin for "migrating redness."

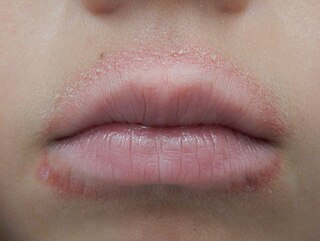
Cheilitis is a medical condition characterized by inflammation of the lips. The inflammation may include the perioral skin, the vermilion border, or the labial mucosa. The skin and the vermilion border are more commonly involved, as the mucosa is less affected by inflammatory and allergic reactions.

Flea allergy dermatitis is an eczematous itchy skin disease of dogs and cats. For both of these domestic species, flea allergy dermatitis is the most common cause of skin disease. Affected animals develop allergic reactions to chemicals in flea saliva. Symptoms of this reaction include erythema (redness), papules (bumps), pustules, and crusts (scabs). If severe, hair loss will occur in the affected area. Dogs with flea allergy dermatitis often show hair loss and eczematous skin rash on the lower back, upper tail, neck, and down the back of the legs. Cats with flea allergy dermatitis may develop a variety of skin problems, including feline eosinophilic granuloma, miliary dermatitis, or self-inflicted alopecia from excessive grooming.

Spongiosis is mainly intercellular edema in the epidermis, and is characteristic of eczematous dermatitis, manifested clinically by intraepidermal vesicles, "juicy" papules, and/or lichenification. It is a severe case of eczema that affects the epidermis, dermis or subcutaneous skin tissues. The three types of spongiotic dermatitis are acute, subacute and chronic. A dermatologist can diagnose acute spongiotic dermatitis by examining the skin during an office visit, but a biopsy is needed for an accurate diagnosis of the type.

Superficial lymphatic malformation is a congenital malformation of the superficial lymphatics, presenting as groups of deep-seated, vesicle-like papules resembling frog spawn, at birth or shortly thereafter. Lymphangioma circumscriptum is the most common congenital lymphatic malformation. It is a benign condition and treatment is not required if the person who has it does not have symptoms from it.

Nickel allergy is any of several allergic conditions provoked by exposure to the chemical element nickel. Nickel allergy often takes the form of nickel allergic contact dermatitis (Ni-ACD), a form of allergic contact dermatitis (ACD). Ni-ACD typically causes a rash that is red and itchy and that may be bumpy or scaly. The main treatment for it is avoiding contact with nickel-releasing metals, such as inexpensive jewelry. Another form of nickel allergy is a systemic form: systemic nickel allergy syndrome (SNAS) can mimic some of the symptoms of irritable bowel syndrome (IBS) and also has a dermatologic component.
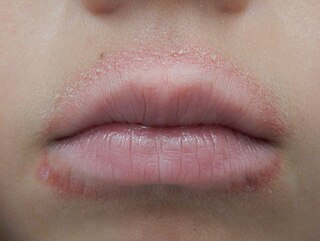
Lip licker's dermatitis is a type of skin inflammation around the lips due to damage by saliva from repetitive lip licking and is classified as a subtype of irritant contact cheilitis. The resulting scaling, redness, chapping, and crusting makes a well-defined ring around the lips. The rash may extend as far as the tongue can reach and usually does not occur at the corners of the mouth. It commonly occurs during winter months but some people can have it year-round if lip licking is a chronic habit.
Two feet-one hand syndrome(TFOHS), is a long-term fungal condition where athlete's foot or fungal toe nail infections in both feet is associated with tinea manuum in one hand. Often the feet are affected for several years before symptoms of a diffuse scaling rash on the palm of one hand appear, which is when most affected people then seek medical help.