Breast cancer is cancer that develops from breast tissue. Signs of breast cancer may include a lump in the breast, a change in breast shape, dimpling of the skin, milk rejection, fluid coming from the nipple, a newly inverted nipple, or a red or scaly patch of skin. In those with distant spread of the disease, there may be bone pain, swollen lymph nodes, shortness of breath, or yellow skin.

Mastitis is inflammation of the breast or udder, usually associated with breastfeeding. Symptoms typically include local pain and redness. There is often an associated fever and general soreness. Onset is typically fairly rapid and usually occurs within the first few months of delivery. Complications can include abscess formation.

Uterine cancer, also known as womb cancer, includes two types of cancer that develop from the tissues of the uterus. Endometrial cancer forms from the lining of the uterus, and uterine sarcoma forms from the muscles or support tissue of the uterus. Endometrial cancer accounts for approximately 90% of all uterine cancers in the United States. Symptoms of endometrial cancer include changes in vaginal bleeding or pain in the pelvis. Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the vagina.

Endometrial cancer is a cancer that arises from the endometrium. It is the result of the abnormal growth of cells that have the ability to invade or spread to other parts of the body. The first sign is most often vaginal bleeding not associated with a menstrual period. Other symptoms include pain with urination, pain during sexual intercourse, or pelvic pain. Endometrial cancer occurs most commonly after menopause.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

Invasive carcinoma of no special type, invasive breast carcinoma of no special type (IBC-NST), invasive ductal carcinoma (IDC), infiltrating ductal carcinoma (IDC) or invasive ductal carcinoma, not otherwise specified (NOS) is a disease. For international audiences this article will use "invasive carcinoma NST" because it is the preferred term of the World Health Organization (WHO).

Ductal carcinoma in situ (DCIS), also known as intraductal carcinoma, is a pre-cancerous or non-invasive cancerous lesion of the breast. DCIS is classified as Stage 0. It rarely produces symptoms or a breast lump one can feel, typically being detected through screening mammography. It has been diagnosed in a significant percentage of men.

Extramammary Paget's disease (EMPD) is a rare and slow-growing malignancy which occurs within the epithelium and accounts for 6.5% of all Paget's disease. The clinical presentation of this disease is similar to the characteristics of mammary Paget's disease (MPD). However, unlike MPD, which occurs in large lactiferous ducts and then extends into the epidermis, EMPD originates in glandular regions rich in apocrine secretions outside the mammary glands. EMPD incidence is increasing by 3.2% every year, affecting hormonally-targeted tissues such as the vulva and scrotum. In women, 81.3% of EMPD cases are related to the vulva, while for men, 43.2% of the manifestations present at the scrotum.
Triple-negative breast cancer (TNBC) is any breast cancer that either lacks or shows low levels of estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor receptor 2 (HER2) overexpression and/or gene amplification. Triple-negative is sometimes used as a surrogate term for basal-like.
Breast cancer management takes different approaches depending on physical and biological characteristics of the disease, as well as the age, over-all health and personal preferences of the patient. Treatment types can be classified into local therapy and systemic treatment. Local therapy is most efficacious in early stage breast cancer, while systemic therapy is generally justified in advanced and metastatic disease, or in diseases with specific phenotypes.

Medullary breast carcinoma is a rare type of breast cancer that is characterized as a relatively circumscribed tumor with pushing, rather than infiltrating, margins. It is histologically characterized as poorly differentiated cells with abundant cytoplasm and pleomorphic high grade vesicular nuclei. It involves lymphocytic infiltration in and around the tumor and can appear to be brown in appearance with necrosis and hemorrhage. Prognosis is measured through staging but can often be treated successfully and has a better prognosis than other infiltrating breast carcinomas.
Metaplastic carcinoma, otherwise known as metaplastic carcinoma of the breast (MCB), is a heterogeneous group of cancers that exhibit varied patterns of metaplasia and differentiation along multiple cell lines. This rare and aggressive form of breast cancer is characterized as being composed of a mixed group of neoplasms containing both glandular and non-glandular patterns with epithelial and/or mesenchymal components. It accounts for fewer than 1% of all breast cancer diagnoses. It is most closely associated with invasive ductal carcinoma of no special type. (IDC), and shares similar treatment approaches. Relative to IDC, MCB generally has higher histological grade and larger tumor size at time of diagnosis, with a lower incidence of axillary lymph node involvement. MCB tumors are typically estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor-2 (HER-2) negative, meaning hormone therapy is generally not an effective treatment option, which correlates to a relatively poor prognosis. MCB was first recognized as a distinct pathological entity in 2000 by the World Health Organization.
The estrogen receptor test (ERT) is a laboratory test to determine whether cancer cells have estrogen receptors. This information can help establish how the cancer should be treated.
Breast cancer classification divides breast cancer into categories according to different schemes criteria and serving a different purpose. The major categories are the histopathological type, the grade of the tumor, the stage of the tumor, and the expression of proteins and genes. As knowledge of cancer cell biology develops these classifications are updated.

Male breast cancer (MBC) is a cancer in males that originates in their breasts. Males account for less than 1% of new breast cancers with about 20,000 new cases being diagnosed worldwide every year. Its incidence rates in males vs. females are, respectively, 0.4 and 66.7 per 100,000 person-years. The worldwide incidences of male as well as female breast cancers have been increasing over the last few decades. Currently, one of every 800 men are estimated to develop this cancer during their lifetimes.
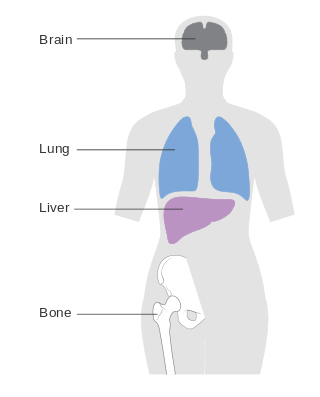
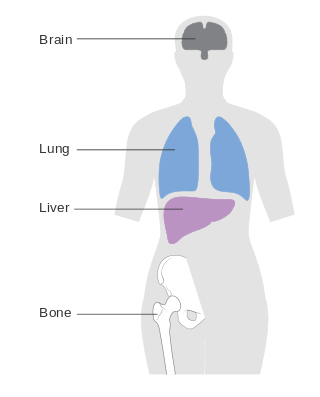
Metastatic breast cancer, also referred to as metastases, advanced breast cancer, secondary tumors, secondaries or stage IV breast cancer, is a stage of breast cancer where the breast cancer cells have spread to distant sites beyond the axillary lymph nodes. There is no cure for metastatic breast cancer; there is no stage after IV.

Gynecomastia is the abnormal non-cancerous enlargement of one or both breasts in males due to the growth of breast tissue as a result of a hormone imbalance between estrogens and androgens. Gynecomastia can cause significant psychological distress or unease.
An estrogen-dependent condition can be that relating to the differentiation in the steroid sex hormone that is associated with the female reproductive system and sex characteristics. These conditions can fall under the umbrella of hypoestrogenism, hyperestrogenim, or any sensitivity to the presence of estrogen in the body.
Endocrine therapy is a common treatment for estrogen receptor positive breast cancer. However, resistance to this therapy can develop, leading to relapse and progression of disease. This highlights the need for new strategies to combat this resistance.

Breast and ovarian cancer does not necessarily imply that both cancers occur at the same time, but rather that getting one cancer would lead to the development of the other within a few years. Women with a history of breast cancer have a higher chance of developing ovarian cancer, vice versa.