
Intracranial epidermoid cysts develop in the early embryonic phases. The cysts develop when epithelial cells are confined with cells that form the brain. [2]

Intracranial epidermoid cysts develop in the early embryonic phases. The cysts develop when epithelial cells are confined with cells that form the brain. [2]
Review of past cases, patients often do not exhibit many symptoms or obtain a diagnosis until they are around 20 to 40 years old. If the patient does show symptoms, it is most likely due to pressure from growth of the tumor. Depending on which part the epidermoid is pressing against can result in varying symptoms.[ citation needed ]
These tumors arise when epidermal cells become trapped during neural tube closure. This occurs between the 3rd to 5th week of fetal development.[ citation needed ]
This section may require cleanup to meet Wikipedia's quality standards. The specific problem is: This section is a hodge-podge.(December 2020) |
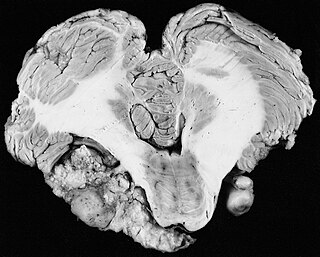
The chances of intracranial epidermoids is about 1% of all brain tumors. This benign tumor of the brain is made up of normal skin cells (stratified epithelial lining) on the outside, and fatty acids and keratin are on the inside of the tumor or sac. Only the sticky outer membrane is alive thus sticking to brain tissues and nerves.
Epidermoid tumors strongly adhere to the brain stem or cranial nerves. Often the lining of the tumor connected to the brain stem or parts difficult to "peel" away are left behind leaving residual tumor after surgery, this can contribute to the risk of regrowth.
About 40% of these cysts originate in the cerebellopontine angle. [3]
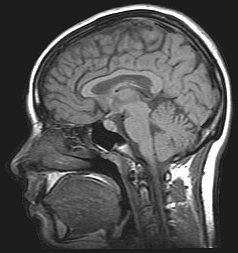
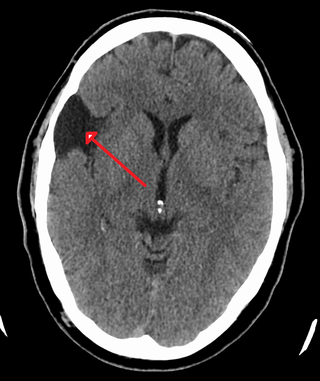
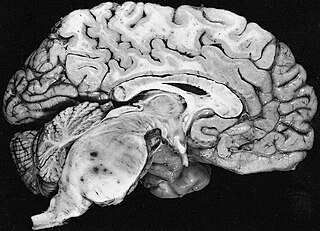
Magnetic resonance imaging (MRI) and computed tomography (CT) brain scans can be used to identify these tumors.[ citation needed ]
Treatment to remove these tumors always involve radical surgery. The reported recurrence rate for a subtotal removal is 30% after a mean interval period of 8.1 years. [4] Surgery is the primary treatment for removal of the brain tumor. Use of an endoscope may assist on obtaining a more complete surgical removal from hidden recesses. [5]
It has been seen that a few patients have tumors that grow unusually fast, especially after surgery. After surgery it is highly suggested the patients get quarterly MRI's to monitor their tumors or as per neurosurgeons/neurologists order. If monitoring the tumor, it is suggested to use the same facility for each scan. Using different facilities can result in minor variations in the scan which can result in false measurements of the brain tumor.[ citation needed ]
Intracranial epidermoid tumors are slow growing lesions, which may recur after incomplete removal during surgery, although it will most likely take many years. These slow growing benign brain tumors envelop nerves and arteries rather than displacing them.[ citation needed ]
Idiopathic intracranial hypertension (IIH), previously known as pseudotumor cerebri and benign intracranial hypertension, is a condition characterized by increased intracranial pressure without a detectable cause. The main symptoms are headache, vision problems, ringing in the ears, and shoulder pain. Complications may include vision loss.

A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant (cancerous) tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

A thymoma is a tumor originating from the epithelial cells of the thymus that is considered a rare malignancy. Thymomas are frequently associated with neuromuscular disorders such as myasthenia gravis; thymoma is found in 20% of patients with myasthenia gravis. Once diagnosed, thymomas may be removed surgically. In the rare case of a malignant tumor, chemotherapy may be used.
A vestibular schwannoma (VS), also called acoustic neuroma, is a benign tumor that develops on the vestibulocochlear nerve that passes from the inner ear to the brain. The tumor originates when Schwann cells that form the insulating myelin sheath on the nerve malfunction. Normally, Schwann cells function beneficially to protect the nerves which transmit balance and sound information to the brain. However, sometimes a mutation in the tumor suppressor gene, NF2, located on chromosome 22, results in abnormal production of the cell protein named Merlin, and Schwann cells multiply to form a tumor. The tumor originates mostly on the vestibular division of the nerve rather than the cochlear division, but hearing as well as balance will be affected as the tumor enlarges.

A prolactinoma is a tumor (adenoma) of the pituitary gland that produces the hormone prolactin. It is the most common type of functioning pituitary tumor. Symptoms of prolactinoma are due to abnormally high levels of prolactin in the blood (hyperprolactinemia), or due to pressure of the tumor on surrounding brain tissue and/or the optic nerves. Based on its size, a prolactinoma may be classified as a microprolactinoma or a macroprolactinoma.

An ependymoma is a tumor that arises from the ependyma, a tissue of the central nervous system. Usually, in pediatric cases the location is intracranial, while in adults it is spinal. The common location of intracranial ependymomas is the fourth ventricle. Rarely, ependymomas can occur in the pelvic cavity.

Meningioma, also known as meningeal tumor, is typically a slow-growing tumor that forms from the meninges, the membranous layers surrounding the brain and spinal cord. Symptoms depend on the location and occur as a result of the tumor pressing on nearby tissue. Many cases never produce symptoms. Occasionally seizures, dementia, trouble talking, vision problems, one sided weakness, or loss of bladder control may occur.

An epidermoid cyst or epidermal inclusion cyst is a benign cyst usually found on the skin. The cyst develops out of ectodermal tissue. Histologically, it is made of a thin layer of squamous epithelium.

Pilocytic astrocytoma is a brain tumor that occurs most commonly in children and young adults. They usually arise in the cerebellum, near the brainstem, in the hypothalamic region, or the optic chiasm, but they may occur in any area where astrocytes are present, including the cerebral hemispheres and the spinal cord. These tumors are usually slow growing and benign, corresponding to WHO malignancy grade 1.

A craniopharyngioma is a rare type of brain tumor derived from pituitary gland embryonic tissue that occurs most commonly in children, but also affects adults. It may present at any age, even in the prenatal and neonatal periods, but peak incidence rates are childhood-onset at 5–14 years and adult-onset at 50–74 years. People may present with bitemporal inferior quadrantanopia leading to bitemporal hemianopsia, as the tumor may compress the optic chiasm. It has a point prevalence around two per 1,000,000. Craniopharyngiomas are distinct from Rathke's cleft tumours and intrasellar arachnoid cysts.

Empty sella syndrome is the condition when the pituitary gland shrinks or becomes flattened, filling the sella turcica with cerebrospinal fluid instead of the normal pituitary. It can be discovered as part of the diagnostic workup of pituitary disorders, or as an incidental finding when imaging the brain.

A colloid cyst is a non-malignant tumor in the brain. It consists of a gelatinous material contained within a membrane of epithelial tissue. It is almost always found just posterior to the foramen of Monro in the anterior aspect of the third ventricle, originating from the roof of the ventricle. Because of its location, it can cause obstructive hydrocephalus and increased intracranial pressure. Colloid cysts represent 0.5–1.0% of intracranial tumors.
The cerebellopontine angle syndrome is a distinct neurological syndrome of deficits that can arise due to the closeness of the cerebellopontine angle to specific cranial nerves. Indications include unilateral hearing loss (85%), speech impediments, disequilibrium, tremors or other loss of motor control. The cerebellopontine angle cistern is a subarachnoid cistern formed by the cerebellopontine angle that lies between the cerebellum and the pons. It is filled with cerebrospinal fluid and is a common site for the growth of acoustic neuromas or schwannomas.

Mollaret's meningitis is a recurrent or chronic inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Since Mollaret's meningitis is a recurrent, benign (non-cancerous), aseptic meningitis, it is also referred to as benign recurrent lymphocytic meningitis. It was named for Pierre Mollaret, the French neurologist who first described it in 1944.
A central nervous system cyst is a type of cyst that presents and affects part of the central nervous system (CNS). They are usually benign and filled with either cerebrospinal fluid, blood, or tumor cells. CNS cysts are classified into two categories: cysts that originate from non-central nervous system tissue, migrate to, and form on a portion of the CNS, and cysts that originate within central nervous system tissue itself. Within these two categories, there are many types of CNS cysts that have been identified from previous studies.
Fibrillary astrocytomas are a group of primary slow-growing brain tumors that typically occur in adults between the ages of 20 and 50.

Subependymal giant cell astrocytoma is a low-grade astrocytic brain tumor (astrocytoma) that arises within the ventricles of the brain. It is most commonly associated with tuberous sclerosis complex (TSC). Although it is a low-grade tumor, its location can potentially obstruct the ventricles and lead to hydrocephalus.

Astroblastoma is a rare glial tumor derived from the astroblast, a type of cell that closely resembles spongioblastoma and astrocytes. Astroblastoma cells are most likely found in the supratentorial region of the brain that houses the cerebrum, an area responsible for all voluntary movements in the body. It also occurs significantly in the frontal lobe, parietal lobe, and temporal lobe, areas where movement, language creation, memory perception, and environmental surroundings are expressed. These tumors can be present in major brain areas not associated with the main cerebral hemispheres, including the cerebellum, optic nerve, cauda equina, hypothalamus, and brain stem.

Aqueductal stenosis is a narrowing of the aqueduct of Sylvius which blocks the flow of cerebrospinal fluid (CSF) in the ventricular system. Blockage of the aqueduct can lead to hydrocephalus, specifically as a common cause of congenital and/or obstructive hydrocephalus.
A central nervous system tumor is an abnormal growth of cells from the tissues of the brain or spinal cord. CNS tumor is a generic term encompassing over 120 distinct tumor types. Common symptoms of CNS tumors include vomiting, headache, changes in vision, nausea, and seizures. A CNS tumor can be detected and classified via neurological examination, medical imaging, such as x-ray imaging, magnetic resonance imaging (MRI) or computed tomography (CT), or after analysis of a biopsy.
[new reference] Mtanda AT; Cruysberg JRM; Merx JL; Thyssen HOM (1986). “The Ocular presentation of intracranial epidermoid tumors. A review of 37 cases from the literature with personal observations in one new patient”. Neuro-ophthalmology. 6(4): 223–230. doi:10.3109/01658108609034219.