Ramsay Hunt syndrome type 2, commonly referred to simply as Ramsay Hunt syndrome (RHS) and also known as herpes zoster oticus, is inflammation of the geniculate ganglion of the facial nerve as a late consequence of varicella zoster virus (VZV). In regard to the frequency, less than 1% of varicella zoster infections involve the facial nerve and result in RHS. It is traditionally defined as a triad of ipsilateral facial paralysis, otalgia, and vesicles close to the ear and auditory canal. Due to its proximity to the vestibulocochlear nerve, the virus can spread and cause hearing loss, tinnitus, and vertigo. It is common for diagnoses to be overlooked or delayed, which can raise the likelihood of long-term consequences. It is more complicated than Bell's palsy. Therapy aims to shorten its overall length, while also providing pain relief and averting any consequences.

Transverse myelitis (TM) is a rare neurological condition wherein the spinal cord is inflamed. The adjective transverse implies that the spinal inflammation (myelitis) extends horizontally throughout the cross section of the spinal cord; the terms partial transverse myelitis and partial myelitis are sometimes used to specify inflammation that affects only part of the width of the spinal cord. TM is characterized by weakness and numbness of the limbs, deficits in sensation and motor skills, dysfunctional urethral and anal sphincter activities, and dysfunction of the autonomic nervous system that can lead to episodes of high blood pressure. Signs and symptoms vary according to the affected level of the spinal cord. The underlying cause of TM is unknown. The spinal cord inflammation seen in TM has been associated with various infections, immune system disorders, or damage to nerve fibers, by loss of myelin. As opposed to leukomyelitis which affects only the white matter, it affects the entire cross-section of the spinal cord. Decreased electrical conductivity in the nervous system can result.

Viral meningitis, also known as aseptic meningitis, is a type of meningitis due to a viral infection. It results in inflammation of the meninges. Symptoms commonly include headache, fever, sensitivity to light and neck stiffness.

Varicella zoster virus (VZV), also known as human herpesvirus 3 or Human alphaherpesvirus 3 (taxonomically), is one of nine known herpes viruses that can infect humans. It causes chickenpox (varicella) commonly affecting children and young adults, and shingles in adults but rarely in children. VZV infections are species-specific to humans. The virus can survive in external environments for a few hours.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.

Shingles, also known as herpes zoster, is a viral disease characterized by a painful skin rash with blisters in a localized area. Typically the rash occurs in a single, wide mark either on the left or right side of the body or face. Two to four days before the rash occurs there may be tingling or local pain in the area. Other common symptoms are fever, headache, and tiredness. The rash usually heals within two to four weeks; however, some people develop ongoing nerve pain which can last for months or years, a condition called postherpetic neuralgia (PHN). In those with poor immune function the rash may occur widely. If the rash involves the eye, vision loss may occur.

Aciclovir, also known as acyclovir, is an antiviral medication. It is primarily used for the treatment of herpes simplex virus infections, chickenpox, and shingles. Other uses include prevention of cytomegalovirus infections following transplant and severe complications of Epstein–Barr virus infection. It can be taken by mouth, applied as a cream, or injected.

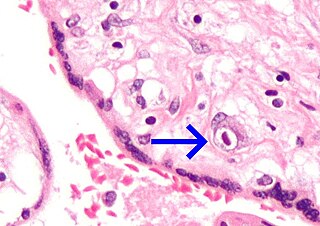
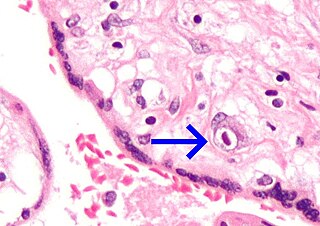
Human polyomavirus 2, commonly referred to as the JC virus or John Cunningham virus, is a type of human polyomavirus. It was identified by electron microscopy in 1965 by ZuRhein and Chou, and by Silverman and Rubinstein, and later isolated in culture and named using the two initials of a patient, John Cunningham, with progressive multifocal leukoencephalopathy (PML). The virus causes PML and other diseases only in cases of immunodeficiency, as in AIDS or during treatment with immunosuppressive drugs.
Postherpetic neuralgia (PHN) is neuropathic pain that occurs due to damage to a peripheral nerve caused by the reactivation of the varicella zoster virus. PHN is defined as pain in a dermatomal distribution that lasts for at least 90 days after an outbreak of herpes zoster. Several types of pain may occur with PHN including continuous burning pain, episodes of severe shooting or electric-like pain, and a heightened sensitivity to gentle touch which would not otherwise cause pain or to painful stimuli. Abnormal sensations and itching may also occur.

Aseptic meningitis is the inflammation of the meninges, a membrane covering the brain and spinal cord, in patients whose cerebral spinal fluid test result is negative with routine bacterial cultures. Aseptic meningitis is caused by viruses, mycobacteria, spirochetes, fungi, medications, and cancer malignancies. The testing for both meningitis and aseptic meningitis is mostly the same. A cerebrospinal fluid sample is taken by lumbar puncture and is tested for leukocyte levels to determine if there is an infection and goes on to further testing to see what the actual cause is. The symptoms are the same for both meningitis and aseptic meningitis but the severity of the symptoms and the treatment can depend on the certain cause.
WHO Disease Staging System for HIV Infection and Disease in Adults and Adolescents was first produced in 1990 by the World Health Organization and updated in September 2005. It is an approach for use in resource limited settings and is widely used in Africa and Asia and has been a useful research tool in studies of progression to symptomatic HIV disease.
A vertically transmitted infection is an infection caused by pathogenic bacteria or viruses that use mother-to-child transmission, that is, transmission directly from the mother to an embryo, fetus, or baby during pregnancy or childbirth. It can occur when the mother has a pre-existing disease or becomes infected during pregnancy. Nutritional deficiencies may exacerbate the risks of perinatal infections. Vertical transmission is important for the mathematical modelling of infectious diseases, especially for diseases of animals with large litter sizes, as it causes a wave of new infectious individuals.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

Genital herpes is a herpes infection of the genitals caused by the herpes simplex virus (HSV). Most people either have no or mild symptoms and thus do not know they are infected. When symptoms do occur, they typically include small blisters that break open to form painful ulcers. Flu-like symptoms, such as fever, aching, or swollen lymph nodes, may also occur. Onset is typically around 4 days after exposure with symptoms lasting up to 4 weeks. Once infected further outbreaks may occur but are generally milder.

Clobetasone (INN) is a corticosteroid used in dermatology, for treating such skin inflammation as seen in eczema, psoriasis and other forms of dermatitis, and ophthalmology. Topical clobetasone butyrate has shown minimal suppression of the hypothalamic–pituitary–adrenal axis.

Mollaret's meningitis is a recurrent or chronic inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Since Mollaret's meningitis is a recurrent, benign (non-cancerous), aseptic meningitis, it is also referred to as benign recurrent lymphocytic meningitis. It was named for Pierre Mollaret, the French neurologist who first described it in 1944.
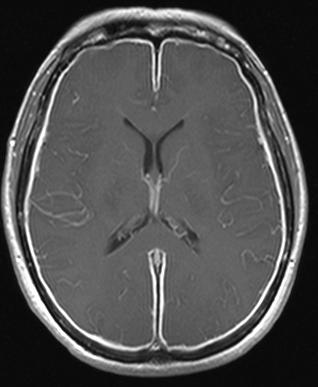
The central nervous system (CNS) controls most of the functions of the body and mind. It comprises the brain, spinal cord and the nerve fibers that branch off to all parts of the body. The CNS viral diseases are caused by viruses that attack the CNS. Existing and emerging viral CNS infections are major sources of human morbidity and mortality.

Chickenpox, or chicken pox, also known as varicella, is a highly contagious, vaccine-preventable disease caused by the initial infection with varicella zoster virus (VZV), a member of the herpesvirus family. The disease results in a characteristic skin rash that forms small, itchy blisters, which eventually scab over. It usually starts on the chest, back, and face. It then spreads to the rest of the body. The rash and other symptoms, such as fever, tiredness, and headaches, usually last five to seven days. Complications may occasionally include pneumonia, inflammation of the brain, and bacterial skin infections. The disease is usually more severe in adults than in children.
Herpes meningitis is inflammation of the meninges, the protective tissues surrounding the spinal cord and brain, due to infection from viruses of the Herpesviridae family - the most common amongst adults is HSV-2. Symptoms are self-limiting over 2 weeks with severe headache, nausea, vomiting, neck-stiffness, and photophobia. Herpes meningitis can cause Mollaret's meningitis, a form of recurrent meningitis. Lumbar puncture with cerebrospinal fluid results demonstrating aseptic meningitis pattern is necessary for diagnosis and polymerase chain reaction is used to detect viral presence. Although symptoms are self-limiting, treatment with antiviral medication may be recommended to prevent progression to Herpes Meningoencephalitis.

Lymphocytic pleocytosis is an abnormal increase in the amount of lymphocytes in the cerebrospinal fluid (CSF). It is usually considered to be a sign of infection or inflammation within the nervous system, and is encountered in a number of neurological diseases, such as pseudomigraine, Susac's syndrome, and encephalitis. While lymphocytes make up roughly a quarter of all white blood cells (WBC) in the body, they are generally rare in the CSF. Under normal conditions, there are usually less than 5 white blood cells per µL of CSF. In a pleocytic setting, the number of lymphocytes can jump to more than 1,000 cells per µL. Increases in lymphocyte count are often accompanied by an increase in cerebrospinal protein concentrations in addition to pleocytosis of other types of white blood cells.