Related Research Articles

Immunology is a branch of medicine and biology that covers the medical study of immune systems in all organisms. In such we can see there is a difference of human immunology and comparative immunology in veterinary medicine and animal biosciences.

A vaccine is a biological preparation that provides active acquired immunity to a particular infectious or malignant disease. The safety and effectiveness of vaccines has been widely studied and verified. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins. The agent stimulates the body's immune system to recognize the agent as a threat, destroy it, and to further recognize and destroy any of the microorganisms associated with that agent that it may encounter in the future.

Immunization, or immunisation, is the process by which an individual's immune system becomes fortified against an infectious agent.
In biology, immunity is the state of being insusceptible or resistant to a noxious agent or process, especially a pathogen or infectious disease. Immunity may occur naturally or be produced by prior exposure or immunization.

In immunology, seroconversion is the development of specific antibodies in the blood serum as a result of infection or immunization, including vaccination. During infection or immunization, antigens enter the blood, and the immune system begins to produce antibodies in response. Before seroconversion, the antigen itself may or may not be detectable, but the antibody is absent. During seroconversion, the antibody is present but not yet detectable. After seroconversion, the antibody is detectable by standard techniques and remains detectable unless the individual seroreverts. Seroreversion, or loss of antibody detectability, can occur due to weakening of the immune system or waning antibody concentration over time. Seroconversion refers the production of specific antibodies against specific antigens, meaning that a single infection could cause multiple waves of seroconversion against different antigens. Similarly, a single antigen could cause multiple waves of seroconversion with different classes of antibodies. For example, most antigens prompt seroconversion for the IgM class of antibodies first, and subsequently the IgG class.
Serology is the scientific study of serum and other body fluids. In practice, the term usually refers to the diagnostic identification of antibodies in the serum. Such antibodies are typically formed in response to an infection, against other foreign proteins, or to one's own proteins. In either case, the procedure is simple.

A conjugate vaccine is a type of subunit vaccine which combines a weak antigen with a strong antigen as a carrier so that the immune system has a stronger response to the weak antigen.

Original antigenic sin, also known as antigenic imprinting, the Hoskins effect, or immunological imprinting, is the propensity of the immune system to preferentially use immunological memory based on a previous infection when a second slightly different version of that foreign pathogen is encountered. This leaves the immune system "trapped" by the first response it has made to each antigen, and unable to mount potentially more effective responses during subsequent infections. Antibodies or T-cells induced during infections with the first variant of the pathogen are subject to repertoire freeze, a form of original antigenic sin.
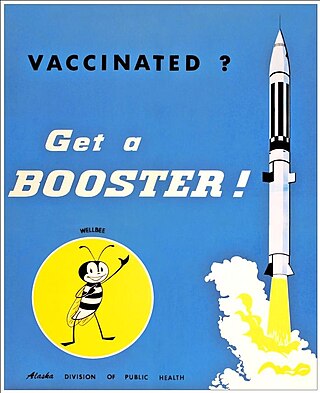
A booster dose is an extra administration of a vaccine after an earlier (primer) dose. After initial immunization, a booster provides a re-exposure to the immunizing antigen. It is intended to increase immunity against that antigen back to protective levels after memory against that antigen has declined through time. For example, tetanus shot boosters are often recommended every 10 years, by which point memory cells specific against tetanus lose their function or undergo apoptosis.
A breakthrough infection is a case of illness in which a vaccinated individual becomes infected with the illness, because the vaccine has failed to provide complete immunity against the pathogen. Breakthrough infections have been identified in individuals immunized against a variety of diseases including mumps, varicella (Chickenpox), influenza, and COVID-19. The characteristics of the breakthrough infection are dependent on the virus itself. Often, infection of the vaccinated individual results in milder symptoms and shorter duration than if the infection were contracted naturally.
In immunology, an adjuvant is a substance that increases or modulates the immune response to a vaccine. The word "adjuvant" comes from the Latin word adiuvare, meaning to help or aid. "An immunologic adjuvant is defined as any substance that acts to accelerate, prolong, or enhance antigen-specific immune responses when used in combination with specific vaccine antigens."

Antibody-dependent enhancement (ADE), sometimes less precisely called immune enhancement or disease enhancement, is a phenomenon in which binding of a virus to suboptimal antibodies enhances its entry into host cells, followed by its replication. The suboptimal antibodies can result from natural infection or from vaccination. ADE may cause enhanced respiratory disease, but is not limited to respiratory disease. It has been observed in HIV, RSV virus and Dengue virus and is monitored for in vaccine development.
Immunization during pregnancy is the administration of a vaccine to a pregnant individual. This may be done either to protect the individual from disease or to induce an antibody response, such that the antibodies cross the placenta and provide passive immunity to the infant after birth. In many countries, including the US, Canada, UK, Australia and New Zealand, vaccination against influenza, COVID-19 and whooping cough is routinely offered during pregnancy.
Gerald Domingue is an American medical researcher and academic who served as Professor of Urology, Microbiology and Immunology in the Tulane University School of Medicine and Graduate School for thirty years and also as Director of Research in Urology. He is currently retired and resides in Zurich, Switzerland, where he is engaged in painting and creative writing. At retirement he was honored with the title of Professor Emeritus at Tulane (1967–1997). Prior to Tulane, he was faculty of Saint Louis University School of Medicine); was a lecturer at Washington University School of Dentistry and director of clinical microbiology in St. Louis City Hospital, St. Louis, Missouri.

The Vaccine Research Center (VRC), is an intramural division of the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), US Department of Health and Human Services (HHS). The mission of the VRC is to discover and develop both vaccines and antibody-based products that target infectious diseases.
As of 2021, a vaccine against Epstein–Barr virus was not yet available. The virus establishes latent infection and causes infectious mononucleosis. There is also increasingly more evidence that EBV may be a trigger of multiple sclerosis. It is a dual-tropic virus, meaning that it infects two different host cell types — in this case, both B cells and epithelial cells. One challenge is that the Epstein–Barr virus expresses very different proteins during its lytic and its latent phases. Antiviral agents act by inhibiting viral DNA replication, but as of 2016, there was little evidence that they are effective against Epstein–Barr virus, they are expensive, they risk causing resistance to antiviral agents, and can cause unpleasant side effects.
A neutralizing antibody (NAb) is an antibody that defends a cell from a pathogen or infectious particle by neutralizing any effect it has biologically. Neutralization renders the particle no longer infectious or pathogenic. Neutralizing antibodies are part of the humoral response of the adaptive immune system against viruses, intracellular bacteria and microbial toxin. By binding specifically to surface structures (antigen) on an infectious particle, neutralizing antibodies prevent the particle from interacting with its host cells it might infect and destroy.

Edward Thomas Ryan is an American microbiologist, immunologist, and physician at Harvard University and Massachusetts General Hospital. Ryan served as president of the American Society of Tropical Medicine and Hygiene from 2009 to 2010. Ryan is Professor of Immunology and Infectious Diseases at the Harvard T.H. Chan School of Public Health, Professor of Medicine at Harvard Medical School, and Director of Global Infectious Diseases at the Massachusetts General Hospital. Ryan's research and clinical focus has been on infectious diseases associated with residing in, immigrating from, or traveling through resource-limited areas. Ryan is a Fellow of the American Society of Microbiology, the American Society of Tropical Medicine and Hygiene, the American College of Physicians, and the Infectious Diseases Society of America.
Immunological memory is the ability of the immune system to quickly and specifically recognize an antigen that the body has previously encountered and initiate a corresponding immune response. Generally, these are secondary, tertiary and other subsequent immune responses to the same antigen. The adaptive immune system and antigen-specific receptor generation are responsible for adaptive immune memory. After the inflammatory immune response to danger-associated antigen, some of the antigen-specific T cells and B cells persist in the body and become long-living memory T and B cells. After the second encounter with the same antigen, they recognize the antigen and mount a faster and more robust response. Immunological memory is the basis of vaccination. Emerging resources show that even the innate immune system can initiate a more efficient immune response and pathogen elimination after the previous stimulation with a pathogen, respectively with PAMPs or DAMPs. Innate immune memory is neither antigen-specific nor dependent on gene rearrangement, but the different response is caused by changes in epigenetic programming and shifts in cellular metabolism. Innate immune memory was observed in invertebrates as well as in vertebrates.
Dan Hung Barouch is an American physician, immunologist, and virologist. He is known for his work on the pathogenesis and immunology of viral infections and the development of vaccine strategies for global infectious diseases.
References
- ↑ Mandavilli, Apoorva (29 August 2020). "Your Coronavirus Test Is Positive. Maybe It Shouldn't Be". The New York Times. Retrieved 8 February 2021.
- ↑ Krueger, Hanna (22 December 2021). "Michael Mina can't stop talking about the need for rapid COVID tests. The country may finally be listening. But is it too late?". Boston Globe. Retrieved 29 December 2021.
- 1 2 Kotlikoff, Laurence; Mina, Michael (3 July 2020). "A Cheap, Simple Way to Control the Coronavirus". The New York Times. Retrieved 8 February 2021.
- 1 2 "2020 Baccalaureate Features Senior Fellow Michael Mina '06". dartmouth.edu. Dartmouth College. 26 May 2020.
- 1 2 "Michael Mina". The Conversation. Retrieved 13 February 2021.
- ↑ "eMed Names Leading Epidemiologist Michael Mina, MD, PhD, as Chief Science Officer". prnewswire.com. 18 November 2021.
- 1 2 "Michael Mina - Bio, Harvard University". Harvard T.H. Chan School of Public Health. Retrieved 11 February 2021.
- 1 2 Frederick, Eva (31 October 2019). "How measles causes the body to 'forget' past infections by other microbes". science.org.
- ↑ "scholar". scholar.google.com. Retrieved 11 February 2021.
- ↑ Larremore DB, Wilder B, Lester E, Shehata S, Burke JM, Hay JA; et al. (2021). "Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening". Sci Adv. 7 (1). Bibcode:2021SciA....7.5393L. doi:10.1126/sciadv.abd5393. PMC 7775777 . PMID 33219112.
{{cite journal}}: CS1 maint: multiple names: authors list (link)