Related Research Articles
General anaesthetics are often defined as compounds that induce a loss of consciousness in humans or loss of righting reflex in animals. Clinical definitions are also extended to include an induced coma that causes lack of awareness to painful stimuli, sufficient to facilitate surgical applications in clinical and veterinary practice. General anaesthetics do not act as analgesics and should also not be confused with sedatives. General anaesthetics are a structurally diverse group of compounds whose mechanisms encompass multiple biological targets involved in the control of neuronal pathways. The precise workings are the subject of some debate and ongoing research.

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.
An antiemetic is a drug that is effective against vomiting and nausea. Antiemetics are typically used to treat motion sickness and the side effects of opioid analgesics, general anaesthetics, and chemotherapy directed against cancer. They may be used for severe cases of gastroenteritis, especially if the patient is dehydrated.

Lidocaine, also known as lignocaine and sold under the brand name Xylocaine among others, is a local anesthetic of the amino amide type. It is also used to treat ventricular tachycardia. When used for local anaesthesia or in nerve blocks, lidocaine typically begins working within several minutes and lasts for half an hour to three hours. Lidocaine mixtures may also be applied directly to the skin or mucous membranes to numb the area. It is often used mixed with a small amount of adrenaline (epinephrine) to prolong its local effects and to decrease bleeding.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients. Depending on the procedure, general anaesthesia may be optional or required. Regardless of whether a patient may prefer to be unconscious or not, certain pain stimuli could result in involuntary responses from the patient that may make an operation extremely difficult. Thus, for many procedures, general anaesthesia is required from a practical perspective.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

An anesthetic or anaesthetic is a drug used to induce anesthesia — in other words, to result in a temporary loss of sensation or awareness. They may be divided into two broad classes: general anesthetics, which result in a reversible loss of consciousness, and local anesthetics, which cause a reversible loss of sensation for a limited region of the body without necessarily affecting consciousness.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory of the experience, it is also possible for victims to have awareness with explicit recall, where they can remember the events related to their surgery.

Bispectral index (BIS) is one of several technologies used to monitor depth of anesthesia. BIS monitors are used to supplement Guedel's classification system for determining depth of anesthesia. Titrating anesthetic agents to a specific bispectral index during general anesthesia in adults allows the anesthetist to adjust the amount of anesthetic agent to the needs of the patient, possibly resulting in a more rapid emergence from anesthesia. Use of the BIS monitor could reduce the incidence of intraoperative awareness during anaesthesia. The exact details of the algorithm used to create the BIS index have not been disclosed by the company that developed it.
Remifentanil, marketed under the brand name Ultiva is a potent, short-acting synthetic opioid analgesic drug. It is given to patients during surgery to relieve pain and as an adjunct to an anaesthetic. Remifentanil is used for sedation as well as combined with other medications for use in general anesthesia. The use of remifentanil has made possible the use of high-dose opioid and low-dose hypnotic anesthesia, due to synergism between remifentanil and various hypnotic drugs and volatile anesthetics.

Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease feeling in a specific area. In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal's epidural space. It is available mixed with a small amount of epinephrine to increase the duration of its action. It typically begins working within 15 minutes and lasts for 2 to 8 hours.
A post-anesthesia care unit (PACU) and sometimes referred to as post-anesthesia recovery or PAR, or simply recovery, is a part of hospitals, ambulatory care centers, and other medical facilities. Patients who received general anesthesia, regional anesthesia, or local anesthesia are transferred from the operating room suites to the recovery area. The patients are monitored typically by anesthesiologists, nurse anesthetists, and other medical staff. Providers follow a standardized handoff to the medical PACU staff that includes, which medications were given in the operating room suites, how hemodynamics were during the procedures, and what is expected for their recovery. After initial assessment and stabilization, patients are monitored for any potential complications, until the patient is transferred back to their hospital rooms.

Droperidol is an antidopaminergic drug used as an antiemetic and as an antipsychotic. Droperidol is also often used as a rapid sedative in intensive-care treatment, and where "agitation aggression or violent behavior" are present.

Levobupivacaine (rINN) is a local anaesthetic drug indicated for minor and major surgical anaesthesia and pain management. It is a long-acting amide-type local anaesthetic that blocks nerve impulses by inhibiting sodium ion influx into the nerve cells. Levobupivacaine is the S-enantiomer of racemic bupivacaine and therefore similar in pharmacological effects. The drug typically starts taking effect within 15 minutes and can last up to 16 hours depending on factors such as site of administration and dosage.
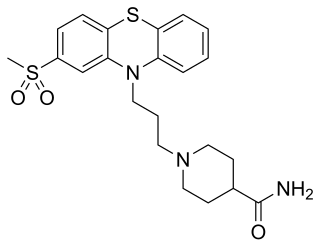
Metopimazine, sold under the brand names Vogalen and Vogalene, is an antiemetic of the phenothiazine group which is used to treat nausea and vomiting. It is marketed in Europe, Canada, and South America. As of August 2020, metopimazine has been repurposed and is additionally under development for use in the United States for the treatment of gastroparesis.
Dental anesthesia is the application of anesthesia to dentistry. It includes local anesthetics, sedation, and general anesthesia.

Twilight anesthesia is an anesthetic technique where a mild dose of sedation is applied to induce anxiolysis, hypnosis, and anterograde amnesia. The patient is not unconscious, but sedated. During surgery or other medical procedures, the patient is under what is known as a "twilight state", where the patient is relaxed and "sleepy", able to follow simple directions by the doctor, and is responsive. Generally, twilight anesthesia causes the patient to forget the surgery and the time right after. It is used for a variety of surgical procedures and for various reasons. Just like regular anesthesia, twilight anesthesia is designed to help a patient feel more comfortable and to minimize pain associated with the procedure being performed and to allow the medical practitioner to practice without interruptions.

Intravenous regional anesthesia (IVRA) or Bier's block anesthesia is an anesthetic technique on the body's extremities where a local anesthetic is injected intravenously and isolated from circulation in a target area. The technique usually involves exsanguination of the target region, which forces blood out of the extremity, followed by the application of pneumatic tourniquets to safely stop blood flow. The anesthetic agent is intravenously introduced into the limb and allowed to diffuse into the surrounding tissue while tourniquets retain the agent within the desired area.

Peter Kranke is anesthetist and professor of anesthesiology at the University of Würzburg, Germany. Kranke is known for the design and conduct of clinical studies and for performing systematic reviews in the context of perioperative medicine. He published numerous papers on research focussed on evidence-based medicine and interventional and observational trials on postoperative nausea and vomiting and other issues in conjunction with perioperative medicine and associated topics including patient blood management. The area of his clinical responsibility and interest, among others, is the safe provision of anesthesia and analgesia in obstetrics and gynecology.
Total intravenous anesthesia (TIVA) refers to the intravenous administration of anesthetic agents to induce a temporary loss of sensation or awareness. The first study of TIVA was done in 1872 using chloral hydrate, and the common anesthetic agent propofol was licensed in 1986. TIVA is currently employed in various procedures as an alternative technique of general anesthesia in order to improve post-operative recovery.
References
- 1 2 3 4 Jewer, James K; Wong, Michael J; Bird, Sally J; Habib, Ashraf S; Parker, Robin; George, Ronald B (29 March 2019). "Supplemental perioperative intravenous crystalloids for postoperative nausea and vomiting". Cochrane Database of Systematic Reviews. 2019 (4): CD012212. doi:10.1002/14651858.CD012212.pub2. PMC 6440702 . PMID 30925195. S2CID 80300081.
- ↑ Nakagawa, Masashi; Kuri, Michioki; Kambara, Noriko; Tanigami, Hironobu; Tanaka, Hideo; Kishi, Yoshihiko; Hamajima, Nobuyuki (February 26, 2008). "Dopamine D2 receptor Taq IA polymorphism is associated with postoperative nausea and vomiting". Journal of Anesthesia. 22 (4): 397–403. doi:10.1007/s00540-008-0661-z. PMID 19011779. S2CID 19342889 – via PubMed.
- ↑ Apfel, Christian C.; Läärä, Esa; Koivuranta, Merja; Greim, Clemens-A.; Roewer, Norbert (September 1999). "A Simplified Risk Score for Predicting Postoperative Nausea and Vomiting". Anesthesiology. 91 (3): 693–700. doi:10.1097/00000542-199909000-00022. PMID 10485781.
- ↑ McCracken, Graham C.; Montgomery, Jane (May 2018). "Postoperative nausea and vomiting after unrestricted clear fluids before day surgery: A retrospective analysis". European Journal of Anaesthesiology. 35 (5): 337–342. doi:10.1097/EJA.0000000000000760. PMID 29232253. S2CID 4486702.
- ↑ Gibbison, Ben; Spencer, Ruth (December 2009). "Post-operative nausea and vomiting". Anaesthesia & Intensive Care Medicine. 10 (12): 583–585. doi:10.1016/j.mpaic.2009.09.006.
- ↑ Weibel, Stephanie; Rücker, Gerta; Eberhart, Leopold HJ; Pace, Nathan L; Hartl, Hannah M; Jordan, Olivia L; Mayer, Debora; Riemer, Manuel; Schaefer, Maximilian S; Raj, Diana; Backhaus, Insa; Helf, Antonia; Schlesinger, Tobias; Kienbaum, Peter; Kranke, Peter (19 October 2020). "Drugs for preventing postoperative nausea and vomiting in adults after general anaesthesia: a network meta-analysis". Cochrane Database of Systematic Reviews. 2020 (11): CD012859. doi:10.1002/14651858.CD012859.pub2. PMC 8094506 . PMID 33075160.
- ↑ Fan, Chin-Fu; Tanhui, Eduardo; Joshi, Sanjoy; Trivedi, Shivang; Hong, Yiyan; Shevde, Ketan (April 1997). "Acupressure Treatment for Prevention of Postoperative Nausea and Vomiting". Anesthesia & Analgesia. 84 (4): 821–825. doi:10.1213/00000539-199704000-00023. PMID 9085965.
- ↑ Samad, K; Afshan, G.; Kamal, R. (February 2003). "Effect of acupressure on postoperative nausea and vomiting in laparoscopic cholecystectomy". Journal of Pakistan Medical Association. 53 (2): 68–72. PMID 12705488.
- ↑ Wongyingsinn, Mingkwan; Peanpanich, Pechprapa; Charoensawan, Sirirat (21 October 2022). "A randomized controlled trial comparing incidences of postoperative nausea and vomiting after laparoscopic cholecystectomy for preoperative intravenous fluid loading, ondansetron, and control groups in a regional hospital setting in a developing country". Medicine. 101 (42): e31155. doi:10.1097/MD.0000000000031155. PMC 9592396 . PMID 36281094.
- ↑ Eberhart, L. H. J.; Morin, A. M.; Wulf, H.; Geldner, G. (November 2002). "Patient preferences for immediate postoperative recovery". British Journal of Anaesthesia. 89 (5): 760–761. doi:10.1093/bja/89.5.760. PMID 12393775.