Related Research Articles

Rubella, also known as German measles or three-day measles, is an infection caused by the rubella virus. This disease is often mild, with half of people not realizing that they are infected. A rash may start around two weeks after exposure and last for three days. It usually starts on the face and spreads to the rest of the body. The rash is sometimes itchy and is not as bright as that of measles. Swollen lymph nodes are common and may last a few weeks. A fever, sore throat, and fatigue may also occur. Joint pain is common in adults. Complications may include bleeding problems, testicular swelling, encephalitis, and inflammation of nerves. Infection during early pregnancy may result in a miscarriage or a child born with congenital rubella syndrome (CRS). Symptoms of CRS manifest as problems with the eyes such as cataracts, deafness, as well as affecting the heart and brain. Problems are rare after the 20th week of pregnancy.

Congenital rubella infection (CRI) occurs when a fetus contracts the rubella virus via maternal-fetal transmission. It can result in various outcomes ranging from asymptomatic infection to congenital defects to miscarriage and fetal death. Congenital rubella syndrome (CRS) refers to a congenital rubella infection that results in various presentations of birth anomalies. If infection occurs 0–11 weeks after conception, the infant has a 90% risk of being affected. If the infection occurs 12–20 weeks after conception, the risk is 20%. Infants are not generally affected if rubella is contracted during the third trimester. Congenital rubella syndrome was discovered in 1941 by Australian Norman McAlister Gregg.

Family planning is the consideration of the number of children a person wishes to have, including the choice to have no children, and the age at which they wish to have them. Things that may play a role on family planning decisions include marital situation, career or work considerations, financial situations. If sexually active, family planning may involve the use of contraception and other techniques to control the timing of reproduction.

Prenatal testing consists of prenatal screening and prenatal diagnosis, which are aspects of prenatal care that focus on detecting problems with the pregnancy as early as possible. These may be anatomic and physiologic problems with the health of the zygote, embryo, or fetus, either before gestation even starts or as early in gestation as practicable. Screening can detect problems such as neural tube defects, chromosome abnormalities, and gene mutations that would lead to genetic disorders and birth defects, such as spina bifida, cleft palate, Down syndrome, Tay–Sachs disease, sickle cell anemia, thalassemia, cystic fibrosis, muscular dystrophy, and fragile X syndrome. Some tests are designed to discover problems which primarily affect the health of the mother, such as PAPP-A to detect pre-eclampsia or glucose tolerance tests to diagnose gestational diabetes. Screening can also detect anatomical defects such as hydrocephalus, anencephaly, heart defects, and amniotic band syndrome.

Pregnancy is the time during which one or more offspring develops (gestates) inside a woman's uterus (womb). A multiple pregnancy involves more than one offspring, such as with twins.

A vaccination schedule is a series of vaccinations, including the timing of all doses, which may be either recommended or compulsory, depending on the country of residence. A vaccine is an antigenic preparation used to produce active immunity to a disease, in order to prevent or reduce the effects of infection by any natural or "wild" pathogen.
Pregnancy options counseling is a form of counseling that provides information and support regarding pregnancy. Women seeking pregnancy options counseling are typically doing so in the case of an unplanned or unintended pregnancy. Limited access to birth control and family planning resources, as well as misuse of birth control are some of the major contributing factors to unintended pregnancies around the world. In 2012, the global rate of unintended pregnancies was estimated to be 40 percent, or eighty-five million pregnancies.
Pre-conception counseling is a meeting with a health-care professional by a woman before attempting to become pregnant. It generally includes a pre-conception risk assessment for any potential complications of pregnancy as well as modifications of risk factors, such as increasing folic acid intake to reduce the risk of neural tube defects and counseling on smoking cessation, alcohol reduction, and medications that may compromise fetal development. Physicians, midwives and baby experts recommend that a woman visit them as soon as the woman is contemplating having a child, and optimally around 3 to 6 months before actual attempts are made to conceive. This time frame allows a woman to better prepare her body for successful conception (fertilization) and pregnancy, and allows her to reduce any health risks which are within her control. Agencies such as the March of Dimes have developed screening tools that healthcare providers can use with their patients. In addition, obstetricians or midwives have developed comprehensive check-lists and assessments for the woman who is planning to become pregnant.
Maternal health is the health of women during pregnancy, childbirth, and the postpartum period. In most cases, maternal health encompasses the health care dimensions of family planning, preconception, prenatal, and postnatal care in order to ensure a positive and fulfilling experience. In other cases, maternal health can reduce maternal morbidity and mortality. Maternal health revolves around the health and wellness of pregnant women, particularly when they are pregnant, at the time they give birth, and during child-raising. WHO has indicated that even though motherhood has been considered as a fulfilling natural experience that is emotional to the mother, a high percentage of women develop health problems and sometimes even die. Because of this, there is a need to invest in the health of women. The investment can be achieved in different ways, among the main ones being subsidizing the healthcare cost, education on maternal health, encouraging effective family planning, and ensuring progressive check up on the health of women with children. Maternal morbidity and mortality particularly affects women of color and women living in low and lower-middle income countries.
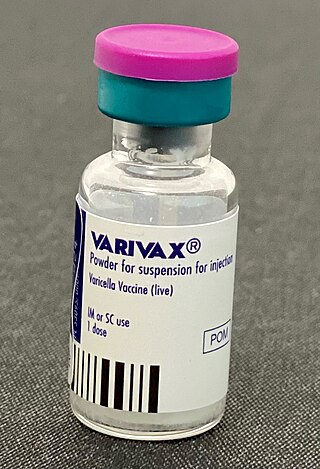
Varicella vaccine, also known as chickenpox vaccine, is a vaccine that protects against chickenpox. One dose of vaccine prevents 95% of moderate disease and 100% of severe disease. Two doses of vaccine are more effective than one. If given to those who are not immune within five days of exposure to chickenpox it prevents most cases of disease. Vaccinating a large portion of the population also protects those who are not vaccinated. It is given by injection just under the skin. Another vaccine, known as zoster vaccine, is used to prevent diseases caused by the same virus – the varicella zoster virus.
Immunization during pregnancy is the administration of a vaccine to a pregnant individual. This may be done either to protect the individual from disease or to induce an antibody response, such that the antibodies cross the placenta and provide passive immunity to the infant after birth. In many countries, including the US, Canada, UK, Australia and New Zealand, vaccination against influenza, COVID-19 and whooping cough is routinely offered during pregnancy.
Long-acting reversible contraceptives (LARC) are methods of birth control that provide effective contraception for an extended period without requiring user action. They include injections, intrauterine devices (IUDs), and subdermal contraceptive implants. They are the most effective reversible methods of contraception because their efficacy is not reliant on patient compliance. The typical use failure rates of IUDs and implants, less than 1% per year, are about the same as perfect use failure rates.

Rubella vaccine is a vaccine used to prevent rubella. Effectiveness begins about two weeks after a single dose and around 95% of people become immune. Countries with high rates of immunization no longer see cases of rubella or congenital rubella syndrome. When there is a low level of childhood immunization in a population it is possible for rates of congenital rubella to increase as more women make it to child-bearing age without either vaccination or exposure to the disease. Therefore, it is important for more than 80% of people to be vaccinated. By introducing rubella containing vaccines, rubella has been eradicated in 81 nations, as of mid-2020.
Unintended pregnancies are pregnancies that are mistimed, unplanned or unwanted at the time of conception.
The following outline is provided as an overview of and topical guide to obstetrics:
Pregnancy when coupled with domestic violence is a form of intimate partner violence (IPV) where health risks may be amplified. Abuse during pregnancy, whether physical, verbal or emotional, produces many adverse physical and psychological effects for both the mother and fetus. Domestic violence during pregnancy is categorized as abusive behavior towards a pregnant woman, where the pattern of abuse can often change in terms of severity and frequency of violence. Abuse may be a long-standing problem in a relationship that continues after a woman becomes pregnant or it may commence in pregnancy. Although female-to-male partner violence occurs in these settings, the overwhelming form of domestic violence is perpetrated by men against women. Pregnancy provides a unique opportunity for healthcare workers to screen women for domestic violence though a recent review found that the best way in which to do this is unclear. Reducing domestic violence in pregnancy should improve outcomes for mothers and babies though more good quality studies are needed to work out effective ways of screening pregnant women.
Prenatal care in the United States is a health care preventive care protocol recommended to women with the goal to provide regular check-ups that allow obstetricians-gynecologists or midwives to detect, treat and prevent potential health problems throughout the course of pregnancy while promoting healthy lifestyles that benefit both mother and child. Patients are encouraged to attend monthly checkups during the first two trimesters and in the third trimester gradually increasing to weekly visits. Women who suspect they are pregnant can schedule pregnancy tests prior to 9 weeks gestation. Once pregnancy is confirmed an initial appointment is scheduled after 8 weeks gestation. Subsequent appointments consist of various tests ranging from blood pressure to glucose levels to check on the health of the mother and fetus. If not, appropriate treatment will then be provided to hinder any further complications.
Reproductive coercion is a collection of behaviors that interfere with decision-making related to reproductive health. These behaviors are meant to maintain power and control related to reproductive health by a current, former, or hopeful intimate or romantic partner, but they can also be perpetrated by parents or in-laws. Coercive behaviors infringe on individuals' reproductive rights and reduce their reproductive autonomy.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.

Maternal healthcare in Texas refers to the provision of family planning services, abortion options, pregnancy-related services, and physical and mental well-being care for women during the prenatal and postpartum periods. The provision of maternal health services in each state can prevent and reduce the incidence of maternal morbidity and mortality and fetal death.
References
- ↑ Hatcher, Robert D. (2011). Contraceptive Technology (20th ed.). Ardent Media, Inc. ISBN 978-1-59708-004-0.
- ↑ James Trussell; Anjana Lalla; Quan Doan; Eileen Reyes; Lionel Pinto; Joseph Gricar (2009). "Cost effectiveness of contraceptives in the United States". Contraception. 79 (1): 5–14. doi:10.1016/j.contraception.2008.08.003. PMC 3638200 . PMID 19041435.
- ↑ Speidel JJ, Harper CC, Shields WC (September 2008). "The potential of long-acting reversible contraception to decrease unintended pregnancy". Contraception. 78 (3): 197–200. doi:10.1016/j.contraception.2008.06.001. PMID 18692608.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Health Care Guideline: Routine Prenatal Care. Fourteenth Edition. Archived 2008-07-05 at the Wayback Machine By the Institute for Clinical Systems Improvement July 2010.
- ↑ Vissenberg, R.; Van Den Boogaard, E.; Van Wely, M.; Van Der Post, J. A.; Fliers, E.; Bisschop, P. H.; Goddijn, M. (2012). "Treatment of thyroid disorders before conception and in early pregnancy: A systematic review". Human Reproduction Update. 18 (4): 360–73. doi: 10.1093/humupd/dms007 . PMID 22431565.
- ↑ Lu, M. C. (2007). "Recommendations for preconception care". American Family Physician. 76 (3): 397–400. PMID 17708141.
- ↑ Faucette, A. N.; Unger, B. L.; Gonik, B.; Chen, K. (2014). "Maternal vaccination: moving the science forward". Human Reproduction Update. 21 (1): 119–135. doi:10.1093/humupd/dmu041. ISSN 1355-4786. PMC 4255605 . PMID 25015234.