Human teeth function to mechanically break down items of food by cutting and crushing them in preparation for swallowing and digesting. As such, they are considered part of the human digestive system. Humans have four types of teeth: incisors, canines, premolars, and molars, which each have a specific function. The incisors cut the food, the canines tear the food and the molars and premolars crush the food. The roots of teeth are embedded in the maxilla or the mandible and are covered by gums. Teeth are made of multiple tissues of varying density and hardness.

Tooth enamel is one of the four major tissues that make up the tooth in humans and many animals, including some species of fish. It makes up the normally visible part of the tooth, covering the crown. The other major tissues are dentin, cementum, and dental pulp. It is a very hard, white to off-white, highly mineralised substance that acts as a barrier to protect the tooth but can become susceptible to degradation, especially by acids from food and drink. In rare circumstances enamel fails to form, leaving the underlying dentin exposed on the surface.

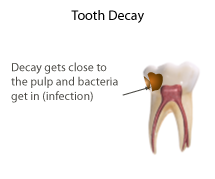
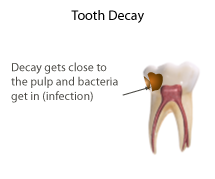
Tooth decay, also known as cavities or caries, is the breakdown of teeth due to acids produced by bacteria. The cavities may be a number of different colors, from yellow to black. Symptoms may include pain and difficulty eating. Complications may include inflammation of the tissue around the tooth, tooth loss and infection or abscess formation. Tooth regeneration is an ongoing stem cell–based field of study that aims to find methods to reverse the effects of decay; current methods are based on easing symptoms.
Dental products are specially fabricated materials, designed for use in dentistry. There are many different types of dental products, and their characteristics vary according to their intended purpose.

Dentin or dentine is a calcified tissue of the body and, along with enamel, cementum, and pulp, is one of the four major components of teeth. It is usually covered by enamel on the crown and cementum on the root and surrounds the entire pulp. By volume, 45% of dentin consists of the mineral hydroxyapatite, 33% is organic material, and 22% is water. Yellow in appearance, it greatly affects the color of a tooth due to the translucency of enamel. Dentin, which is less mineralized and less brittle than enamel, is necessary for the support of enamel. Dentin rates approximately 3 on the Mohs scale of mineral hardness. There are two main characteristics which distinguish dentin from enamel: firstly, dentin forms throughout life; secondly, dentin is sensitive and can become hypersensitive to changes in temperature due to the sensory function of odontoblasts, especially when enamel recedes and dentin channels become exposed.

Endodontics is the dental specialty concerned with the study and treatment of the dental pulp.

The pulp is the connective tissue, nerves, blood vessels, and odontoblasts that comprise the innermost layer of a tooth. The pulp's activity and signalling processes regulate its behaviour.

Deciduous teeth or primary teeth, also informally known as baby teeth, milk teeth, or temporary teeth, are the first set of teeth in the growth and development of humans and other diphyodonts, which include most mammals but not elephants, kangaroos, or manatees, which are polyphyodonts. Deciduous teeth develop during the embryonic stage of development and erupt during infancy. They are usually lost and replaced by permanent teeth, but in the absence of their permanent replacements, they can remain functional for many years into adulthood.

Dentinogenesis imperfecta (DI) is a genetic disorder of tooth development. It is inherited in an autosomal dominant pattern, as a result of mutations on chromosome 4q21, in the dentine sialophosphoprotein gene (DSPP). It is one of the most frequently occurring autosomal dominant features in humans. Dentinogenesis imperfecta affects an estimated 1 in 6,000-8,000 people.
Dens invaginatus (DI), also known as tooth within a tooth, is a rare dental malformation and a developmental anomaly where there is an infolding of enamel into dentin. The prevalence of this condition is 0.3 - 10%, affecting males more frequently than females. The condition presents in two forms, coronal involving tooth crown and radicular involving tooth root, with the former being more common.
Dens evaginatus is a rare odontogenic developmental anomaly that is found in teeth where the outer surface appears to form an extra bump or cusp.

Root canal treatment is a treatment sequence for the infected pulp of a tooth that is intended to result in the elimination of infection and the protection of the decontaminated tooth from future microbial invasion. Root canals, and their associated pulp chamber, are the physical hollows within a tooth that are naturally inhabited by nerve tissue, blood vessels and other cellular entities.
Mineral trioxide aggregate (MTA) is an alkaline, cementitious dental repair material. MTA is used for creating apical plugs during apexification, repairing root perforations during root canal therapy, and treating internal root resorption. It can be used for root-end filling material and as pulp capping material. It has better pulpotomy outcomes than calcium hydroxide or formocresol, and may be the best known material, as of 2018 data. For pulp capping, it has a success rate higher than calcium hydroxide, and indistinguishable from Biodentin.
Pulpotomy is a minimally invasive procedure performed in children on a primary tooth with extensive caries but without evidence of root pathology. The minimally invasive, endodontic techniques of vital pulp therapy (VPT) are based on improved understanding of the capacity of pulp tissues to heal and regenerate plus the availability of advanced endodontic materials. During caries removal, this results in a carious or mechanical pulp exposure from the cavity. During pulpotomy, the inflamed/diseased pulp tissue is removed from the coronal pulp chamber of the tooth, leaving healthy pulp tissue which is dressed with a long-term clinically successful medicament that maintains the survival of the pulp and promotes repair. There are various types of medicament placed above the vital pulp such as Buckley's Solution of formocresol, ferric sulfate, calcium hydroxide or mineral trioxide aggregate (MTA). MTA is a more recent material used for pulpotomies with a high rate of success, better than formocresol or ferric sulfate. It is also recommended to be the preferred pulpotomy agent in the future. After the coronal pulp chamber is filled, the tooth is restored with a filling material that seals the tooth from microleakage, such as a stainless steel crown which is the most effective long-term restoration. However, if there is sufficient remaining supporting tooth structure, other filling materials such as amalgam or composite resin can provide a functional alternative when the primary tooth has a life span of two years or less. The medium- to long-term treatment outcomes of pulpotomy in symptomatic permanent teeth with caries, especially in young people, indicate that pulpotomy can be a potential alternative to root canal therapy (RCT).
Pulp necrosis is a clinical diagnostic category indicating the death of cells and tissues in the pulp chamber of a tooth with or without bacterial invasion. It is often the result of many cases of dental trauma, caries and irreversible pulpitis.

Pulp stones are nodular, calcified masses appearing in either or both the coronal and root portion of the pulp organ in teeth. Pulp stones are not painful unless they impinge on nerves.

Regenerative endodontic procedures is defined as biologically based procedures designed to replace damaged structures such as dentin, root structures, and cells of the pulp-dentin complex. This new treatment modality aims to promote normal function of the pulp. It has become an alternative to heal apical periodontitis. Regenerative endodontics is the extension of root canal therapy. Conventional root canal therapy cleans and fills the pulp chamber with biologically inert material after destruction of the pulp due to dental caries, congenital deformity or trauma. Regenerative endodontics instead seeks to replace live tissue in the pulp chamber. The ultimate goal of regenerative endodontic procedures is to regenerate the tissues and the normal function of the dentin-pulp complex.
Biofilling, also known as the orthograde canal grafting technique or 4D sealing, is an endodontic root canal obturation technique with a Bioceramic material after root canal preparation and enlargement procedure.
An endodontic crown or endocrown is a single prostheses fabricated from reinforced ceramics, indicated for endodontically treated molar teeth that have significant loss of coronal structure. Endocrowns are formed from a monoblock containing the coronal portion invaded in the apical projection that fills the pulp chamber space, and possibly the root canal entrances; they have the advantage of removing lower amounts of sound tissue compared to other techniques, and with much lower chair time needed. They are luted to the tooth structure by an adhesive material. The ceramic can be milled using computer-aided techniques or molded under pressure. Endocrowns can be an alternative to conventional crown restorations.
Apexification is a method of dental treatment to induce a calcific barrier in a root with incomplete formation or open apex of a tooth with necrotic pulp. Pulpal involvement usually occurs as a consequence of trauma or caries involvement of young or immature permanent teeth. As a sequelae of untreated pulp involvement, loss of pulp vitality or necrotic pulp took place for the involved teeth.