A urinary tract infection (UTI) is an infection that affects part of the urinary tract. When it affects the lower urinary tract it is known as a bladder infection (cystitis) and when it affects the upper urinary tract it is known as a kidney infection (pyelonephritis). Symptoms from a lower urinary tract infection include pain with urination, frequent urination, and feeling the need to urinate despite having an empty bladder. Symptoms of a kidney infection include fever and flank pain usually in addition to the symptoms of a lower UTI. Rarely the urine may appear bloody. In the very old and the very young, symptoms may be vague or non-specific.

In urinary catheterization a latex, polyurethane, or silicone tube known as a urinary catheter is inserted into the bladder through the urethra. Catheterization allows urine to drain from the bladder for collection. It may also be used to inject liquids used for treatment or diagnosis of bladder conditions. A clinician, often a nurse, usually performs the procedure, but self-catheterization is also possible. A catheter may be in place for long periods of time or removed after each use.

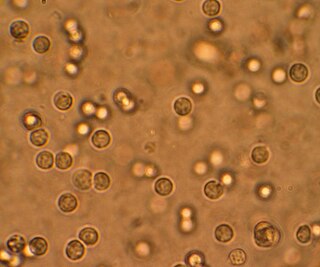
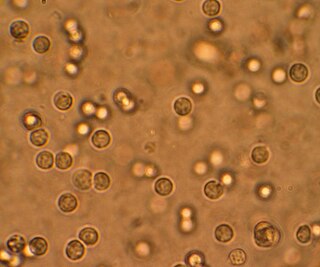
Clinical urine tests are examinations of the physical and chemical properties of urine and its microscopic appearance to aid in medical diagnosis. The term urinalysis—a blend of the words urine and analysis—generally refers to the gross examination of the urine, chemical evaluation using urine test strips, and microscopic examination. Gross examination targets parameters that can be measured with the naked eye, including volume, color, transparency, odor, and specific gravity; urine test strips measure chemical properties such as pH, glucose concentration, and protein levels; and light microscopy is performed to identify elements such as cells, urinary casts, crystals, and organisms. Other analyses routinely performed on urine samples include urine electrolyte levels, drug testing, pregnancy testing and microbiological culture.

Hematuria or haematuria is defined as the presence of blood or red blood cells in the urine. An anatomical framework is helpful in developing a comprehensive differential diagnosis. Blood or red blood cells can enter and mix with urine at multiple anatomical sites. These include the urinary system, female reproductive system, and integumentary system.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.
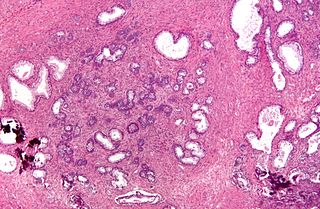
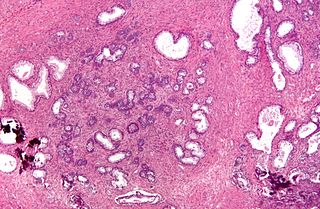
Transurethral resection of the prostate is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, it is performed by visualising the prostate through the urethra and removing tissue by electrocautery or sharp dissection. It has been the standard treatment for BPH for many years, but recently alternative, minimally invasive techniques have become available. This procedure is done with spinal or general anaesthetic. A triple lumen catheter is inserted through the urethra to irrigate and drain the bladder after the surgical procedure is complete. Outcome is considered excellent for 80–90% of BPH patients. The procedure carries minimal risk for erectile dysfunction, moderate risk for bleeding, and a large risk for retrograde ejaculation.

Pyelonephritis is inflammation of the kidney, typically due to a bacterial infection. Symptoms most often include fever and flank tenderness. Other symptoms may include nausea, burning with urination, and frequent urination. Complications may include pus around the kidney, sepsis, or kidney failure.

In urology, a Foley catheter is a flexible tube that a clinician passes through the urethra and into the bladder to drain urine. It is the most common type of indwelling urinary catheter.
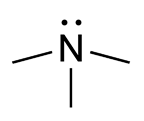
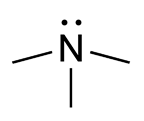
Trimethylaminuria (TMAU), also known as fish odor syndrome or fish malodor syndrome, is a rare metabolic disorder that causes a defect in the normal production of an enzyme named flavin-containing monooxygenase 3 (FMO3). When FMO3 is not working correctly or if not enough enzyme is produced, the body loses the ability to properly convert trimethylamine (TMA) from precursor compounds in food digestion into trimethylamine oxide (TMAO), through a process called N-oxidation. Trimethylamine then builds up and is released in the person's sweat, urine, and breath, giving off a strong fishy odor or strong body odor. A variant of TMAU exists where there is no genetic cause, yet excessive TMA is secreted, possibly due to intestinal dysbiosis, altered metabolism, or hormonal causes.
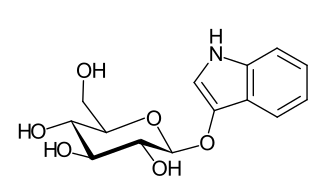
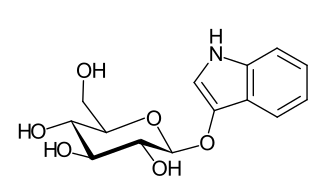
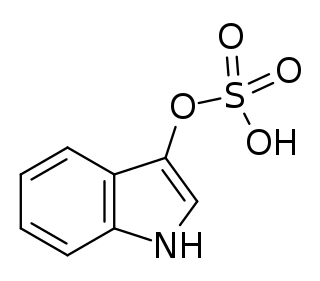
Indican is a colourless organic compound, soluble in water, naturally occurring in Indigofera plants. It is a precursor of indigo dye.
An Indiana pouch is a surgically-created urinary diversion used to create a way for the body to store and eliminate urine for patients who have had their urinary bladders removed as a result of bladder cancer, pelvic exenteration, bladder exstrophy or who are not continent due to a congenital, neurogenic bladder. This particular urinary diversion results in a continent reservoir that the patient must catheterize to empty urine. This concept and technique was developed by Drs. Mike Mitchell, Randall Rowland, and Richard Bihrle at Indiana University.
Neurogenic bladder dysfunction, or neurogenic bladder, refers to urinary bladder problems due to disease or injury of the central nervous system or peripheral nerves involved in the control of urination. There are multiple types of neurogenic bladder depending on the underlying cause and the symptoms. Symptoms include overactive bladder, urinary urgency, frequency, incontinence or difficulty passing urine. A range of diseases or conditions can cause neurogenic bladder including spinal cord injury, multiple sclerosis, stroke, brain injury, spina bifida, peripheral nerve damage, Parkinson's disease, or other neurodegenerative diseases. Neurogenic bladder can be diagnosed through a history and physical as well as imaging and more specialized testing. Treatment depends on underlying disease as well as symptoms and can be managed with behavioral changes, medications, surgeries, or other procedures. The symptoms of neurogenic bladder, especially incontinence, can have a significant impact on quality of life.

Overactive bladder (OAB) is a condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a person's life. The frequent need to urinate may occur during the day, at night, or both. If there is loss of bladder control then it is known as urge incontinence. More than 40% of people with overactive bladder have incontinence. Conversely, about 40% to 70% of urinary incontinence is due to overactive bladder. Overactive bladder is not life-threatening, but most people with the condition have problems for years.

Acute prostatitis is a serious bacterial infection of the prostate gland. This infection is a medical emergency. It should be distinguished from other forms of prostatitis such as chronic bacterial prostatitis and chronic pelvic pain syndrome (CPPS).
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Providencia stuartii, is a Gram negative bacillus that is commonly found in soil, water, and sewage. P. stuartii is the most common of the 5 species found in the genus Providencia, with Providencia rettgeri, Providencia alcalifaciens, Providencia rustigianii, P heimbachae. Providencia stuartii can be incubated at 37 °C in nutrient agar or nutrient broth. P. stuartii is the genomic source for the restriction endonuclease, PstI. Some other important information about P. stuartii is that it is motile via flagella, non-sporulating, non-lactose fermenting, catalase positive and oxidase negative. It can also grow in anaerobic conditions and on Simmon’s Citrate Agar.
Dyssynergia is any disturbance of muscular coordination, resulting in uncoordinated and abrupt movements. This is also an aspect of ataxia. It is typical for dyssynergic patients to split a movement into several smaller movements. Types of dyssynergia include Ramsay Hunt syndrome type 1, bladder sphincter dyssynergia, and anal sphincter dyssynergia.

Emphysematous cystitis is a rare type of infection of the bladder wall by gas-forming bacteria or fungi. The most frequent offending organism is E. coli. Other gram negative bacteria, including Klebsiella and Proteus are also commonly isolated. Fungi, such as Candida, have also been reported as causative organisms. Citrobacter and Enterococci have also been found to cause emphysematous cystitis. Although it is a rare type of bladder infection, it is the most common type of all gas-forming bladder infections. The condition is characterized by the formation of air bubbles in and around the bladder wall. The gas found in the bladder consists of nitrogen, hydrogen, oxygen, and carbon dioxide. The disease most commonly affects elderly diabetic and immunocompromised patients. The first case was identified in a post-mortem examination in 1888.

Indirubin is a chemical compound most often produced as a byproduct of bacterial metabolism. For instance, it is one of the compounds responsible for the generally benign condition purple urine bag syndrome, resulting from bacteria metabolizing indoxyl sulfate found naturally in urine.
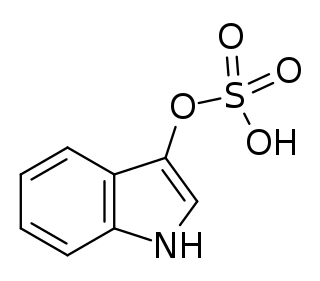
Indoxyl sulfate, also known as 3-indoxylsulfate and 3-indoxylsulfuric acid, is a metabolite of dietary L-tryptophan that acts as a cardiotoxin and uremic toxin. High concentrations of indoxyl sulfate in blood plasma are known to be associated with the development and progression of chronic kidney disease and vascular disease in humans. As a uremic toxin, it stimulates glomerular sclerosis and renal interstitial fibrosis.