Hypertension, also known as high blood pressure, is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure usually does not cause symptoms. It is, however, a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia. Hypertension is a major cause of premature death worldwide.

The Mediterranean diet is a diet inspired by the eating habits and traditional food typical of southern Spain, southern Italy, and Crete, and formulated in the early 1960s. It is distinct from Mediterranean cuisine, which covers the actual cuisines of the Mediterranean countries. While inspired by a specific time and place, the "Mediterranean diet" was later refined based on the results of multiple scientific studies.

Cardiovascular disease (CVD) is any disease involving the heart or blood vessels. CVDs constitute a class of diseases that includes: coronary artery diseases, heart failure, hypertensive heart disease, rheumatic heart disease, cardiomyopathy, arrhythmia, congenital heart disease, valvular heart disease, carditis, aortic aneurysms, peripheral artery disease, thromboembolic disease, and venous thrombosis.
Essential hypertension is the form of hypertension that by definition has no identifiable secondary cause. It is the most common type affecting 85% of those with high blood pressure. The remaining 15% is accounted for by various causes of secondary hypertension. Primary hypertension tends to be familial and is likely to be the consequence of an interaction between environmental and genetic factors. Prevalence of essential hypertension increases with age, and individuals with relatively high blood pressure at younger ages are at increased risk for the subsequent development of hypertension. Hypertension can increase the risk of cerebral, cardiac, and renal events.

Thiazide refers to both a class of sulfur-containing organic molecules and a class of diuretics based on the chemical structure of benzothiadiazine. The thiazide drug class was discovered and developed at Merck and Co. in the 1950s. The first approved drug of this class, chlorothiazide, was marketed under the trade name Diuril beginning in 1958. In most countries, thiazides are the least expensive antihypertensive drugs available.

A healthy diet is a diet that maintains or improves overall health. A healthy diet provides the body with essential nutrition: fluid, macronutrients such as protein, micronutrients such as vitamins, and adequate fibre and food energy.

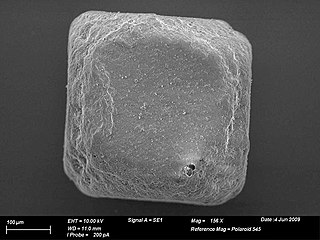
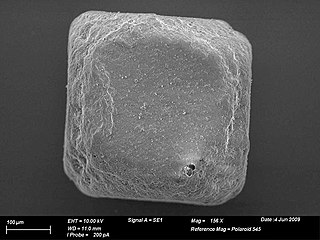
In common usage, salt is a mineral composed primarily of sodium chloride (NaCl). When used in food, especially at table in ground form in dispensers, it is more formally called table salt. In the form of a natural crystalline mineral, salt is also known as rock salt or halite. Salt is essential for life in general, and saltiness is one of the basic human tastes. Salt is one of the oldest and most ubiquitous food seasonings, and is known to uniformly improve the taste perception of food, including otherwise unpalatable food. Salting, brining, and pickling are also ancient and important methods of food preservation.
The DASH diet is a dietary pattern promoted by the U.S.-based National Heart, Lung, and Blood Institute to prevent and control hypertension. The DASH diet is rich in fruits, vegetables, whole grains, and low-fat dairy foods. It includes meat, fish, poultry, nuts, and beans, and is limited in sugar-sweetened foods and beverages, red meat, and added fats. In addition to its effect on blood pressure, it is designed to be a well-balanced approach to eating for the general public. DASH is recommended by the United States Department of Agriculture (USDA) as a healthy eating plan. The DASH diet is one of three healthy diets recommended in the 2015–2020 US Dietary Guidelines, which also include the Mediterranean diet and a vegetarian diet. The American Heart Association (AHA) considers the DASH diet "specific and well-documented across age, sex and ethnically diverse groups."

A salt substitute, also known as low-sodium salt, is a low-sodium alternative to edible salt marketed to reduce the risk of high blood pressure and cardiovascular disease associated with a high intake of sodium chloride while maintaining a similar taste.
The INTERSALT Study was a 1988 international observational study which investigated the link between dietary salt, as measured by urinary excretion, and blood pressure. The study was based on a sample of 10,079 men and women aged 20–59 sampled from 52 populations around the world. The authors of the study attempted to provide a widespread international investigation of the correlation between dietary salt intake and blood pressure in a systematic and standardized way with regards for relevant confounding variables, beyond just age and sex.
Prehypertension, also known as high normal blood pressure and borderline hypertensive (BH), is a medical classification for cases where a person's blood pressure is elevated above optimal or normal, but not to the level considered hypertension. Prehypertension is now referred to as "elevated blood pressure" by the American College of Cardiology (ACC) and the American Heart Association (AHA). The ACC/AHA define elevated blood pressure as readings with a systolic pressure from 120 to 129 mm Hg and a diastolic pressure under 80 mm Hg, and the European Society of Cardiology and European Society of Hypertension (ESC/ESH) define "high normal blood pressure" as readings with a systolic pressure from 130 to 139 mm Hg and a diastolic pressure 85-89 mm Hg. Readings greater than or equal to 130/80 mm Hg are considered hypertension by ACC/AHA and if greater than or equal to 140/90 mm Hg by ESC/ESH.
A low sodium diet is a diet that includes no more than 1,500 to 2,400 mg of sodium per day.
On October 25, 2007, the Minister of Health announced that the Government of Canada would establish an expert Sodium Working Group to explore options for reducing sodium intake and cardiovascular disease among Canadians.
Canadian health claims by Health Canada, the department of the Government of Canada responsible for national health, has allowed five scientifically verified disease risk reduction claims to be used on food labels and on food advertising. Other countries, including the United States and Great Britain, have approved similar health claims on food labels.
The African Society of Hypertension (AfSoH) Initiative is an international organization initiative with the objective to create the African Society of Hypertension with a main goal of providing a stable and organized African platform for scientific exchange in arterial hypertension. The AfSoH Initiative was created in 2010 by the consortium of health professionals and researchers active in field of arterial hypertension on African continent led by Marc Twagirumukiza. The official membership is obtained after registration.
The health effects of salt are the conditions associated with the consumption of either too much or too little salt. Salt is a mineral composed primarily of sodium chloride (NaCl) and is used in food for both preservation and flavor. Sodium ions are needed in small quantities by most living things, as are chloride ions. Salt is involved in regulating the water content of the body. The sodium ion itself is used for electrical signaling in the nervous system.
Hypertension is managed using lifestyle modification and antihypertensive medications. Hypertension is usually treated to achieve a blood pressure of below 140/90 mmHg to 160/100 mmHg. According to one 2003 review, reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34% and of ischaemic heart disease by 21% and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.
Cheryl Ann Marie Anderson is an American epidemiologist. Anderson is a professor at and founding Dean of the University of California San Diego Herbert Wertheim School of Public Health and Human Longevity Science. Anderson's research focus is on nutrition and chronic disease prevention in under-served human populations.
A renal diet is a diet aimed at keeping levels of fluids, electrolytes, and minerals balanced in the body in individuals with chronic kidney disease or who are on dialysis. Dietary changes may include the restriction of fluid intake, protein, and electrolytes including sodium, phosphorus, and potassium. Calories may also be supplemented if the individual is losing weight undesirably.
A non-pharmaceutical intervention or non-pharmacological intervention (NPI) is any type of health intervention which is not primarily based on medication. Some examples include exercise, sleep improvement, or dietary habits.