In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

The tibia, also known as the shinbone or shankbone, is the larger, stronger, and anterior (frontal) of the two bones in the leg below the knee in vertebrates ; it connects the knee with the ankle. The tibia is found on the medial side of the leg next to the fibula and closer to the median plane. The tibia is connected to the fibula by the interosseous membrane of leg, forming a type of fibrous joint called a syndesmosis with very little movement. The tibia is named for the flute tibia. It is the second largest bone in the human body, after the femur. The leg bones are the strongest long bones as they support the rest of the body.

The fibula or calf bone is a leg bone on the lateral side of the tibia, to which it is connected above and below. It is the smaller of the two bones and, in proportion to its length, the most slender of all the long bones. Its upper extremity is small, placed toward the back of the head of the tibia, below the knee joint and excluded from the formation of this joint. Its lower extremity inclines a little forward, so as to be on a plane anterior to that of the upper end; it projects below the tibia and forms the lateral part of the ankle joint.
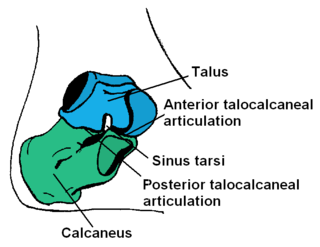
The ankle, the talocrural region or the jumping bone (informal) is the area where the foot and the leg meet. The ankle includes three joints: the ankle joint proper or talocrural joint, the subtalar joint, and the inferior tibiofibular joint. The movements produced at this joint are dorsiflexion and plantarflexion of the foot. In common usage, the term ankle refers exclusively to the ankle region. In medical terminology, "ankle" can refer broadly to the region or specifically to the talocrural joint.
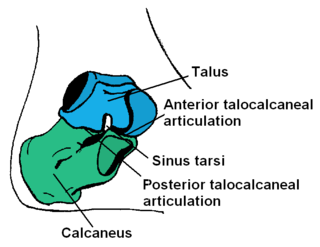
In humans and many other primates, the calcaneus or heel bone is a bone of the tarsus of the foot which constitutes the heel. In some other animals, it is the point of the hock.
An osteotomy is a surgical operation whereby a bone is cut to shorten or lengthen it or to change its alignment. It is sometimes performed to correct a hallux valgus, or to straighten a bone that has healed crookedly following a fracture. It is also used to correct a coxa vara, genu valgum, and genu varum. The operation is done under a general anaesthetic.

The posterior cruciate ligament (PCL) is a ligament in each knee of humans and various other animals. It works as a counterpart to the anterior cruciate ligament (ACL). It connects the posterior intercondylar area of the tibia to the medial condyle of the femur. This configuration allows the PCL to resist forces pushing the tibia posteriorly relative to the femur.

The Maisonneuve fracture is a spiral fracture of the proximal third of the fibula associated with a tear of the distal tibiofibular syndesmosis and the interosseous membrane. There is an associated fracture of the medial malleolus or rupture of the deep deltoid ligament of the ankle. This type of injury can be difficult to detect.

The Segond fracture is a type of avulsion fracture from the lateral tibial plateau of the knee, immediately below the articular surface of the tibia.
The medial collateral ligament (MCL), also called the superficial medial collateral ligament (sMCL) or tibial collateral ligament (TCL), is one of the major ligaments of the knee. It is on the medial (inner) side of the knee joint and occurs in humans and other primates. Its primary function is to resist valgus forces on the knee.
The knee examination, in medicine and physiotherapy, is performed as part of a physical examination, or when a patient presents with knee pain or a history that suggests a pathology of the knee joint.

The unhappy triad, also known as a blown knee among other names, is an injury to the anterior cruciate ligament, medial collateral ligament, and meniscus. Analysis during the 1990s indicated that this 'classic' O'Donoghue triad is actually an unusual clinical entity among athletes with knee injuries. Some authors mistakenly believe that in this type of injury, "combined anterior cruciate and medial collateral ligament disruptions that were incurred during athletic endeavors" always present with concomitant medial meniscus injury. However, the 1990 analysis showed that lateral meniscus tears are more common than medial meniscus tears in conjunction with sprains of the ACL.

A tear of a meniscus is a rupturing of one or more of the fibrocartilage strips in the knee called menisci. When doctors and patients refer to "torn cartilage" in the knee, they actually may be referring to an injury to a meniscus at the top of one of the tibiae. Menisci can be torn during innocuous activities such as walking or squatting. They can also be torn by traumatic force encountered in sports or other forms of physical exertion. The traumatic action is most often a twisting movement at the knee while the leg is bent. In older adults, the meniscus can be damaged following prolonged 'wear and tear'. Especially acute injuries can lead to displaced tears which can cause mechanical symptoms such as clicking, catching, or locking during motion of the joint. The joint will be in pain when in use, but when there is no load, the pain goes away.
A bumper fracture is a fracture of the lateral tibial plateau caused by the bumper of a car coming into contact with the outer side of the knee when a person is standing. Specifically, it is caused by a forced valgus applied to the knee. This causes the lateral part of the distal femur and the lateral tibial plateau to come into contact, compressing the tibial plateau and causing the tibia to fracture. The name of the injury is because it was described as being caused by the impact of a car bumper on the lateral side of the knee while the foot is planted on the ground, although this mechanism is only seen in about 25% of tibial plateau fractures.

A crus fracture is a fracture of the lower legs bones meaning either or both of the tibia and fibula.
Posterolateral corner injuries of the knee are injuries to a complex area formed by the interaction of multiple structures. Injuries to the posterolateral corner can be debilitating to the person and require recognition and treatment to avoid long term consequences. Injuries to the PLC often occur in combination with other ligamentous injuries to the knee; most commonly the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). As with any injury, an understanding of the anatomy and functional interactions of the posterolateral corner is important to diagnosing and treating the injury.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:
The anterolateral ligament (ALL) is a ligament on the lateral aspect of the human knee, anterior to the fibular collateral ligament.
High tibial osteotomy is an orthopaedic surgical procedure which aims to correct a varus deformation with compartmental osteoarthritis. Since the inception of the procedure, advancements to technique, fixation devices, and a better understanding of patient selection has allowed HTO to become more popular in younger, more active patients hoping to combat arthritis. The idea behind the procedure is to realign the weight-bearing line of the knee. By realigning the knee, the force produced from weight-bearing is shifted from the arthritic, medial compartment to the healthy, lateral compartment. This decrease in force or load in the diseased part of the knee joint decreases knee pain and can delay the development or progression of osteoarthritis in the medial compartment.
In the skeleton of humans and other animals, a tubercle, tuberosity or apophysis is a protrusion or eminence that serves as an attachment for skeletal muscles. The muscles attach by tendons, where the enthesis is the connective tissue between the tendon and bone. A tuberosity is generally a larger tubercle.