Related Research Articles

The prostate is both an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found only in some mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue as well as connective tissue.

Benign prostatic hyperplasia (BPH), also called prostate enlargement, is a noncancerous increase in size of the prostate gland. Symptoms may include frequent urination, trouble starting to urinate, weak stream, inability to urinate, or loss of bladder control. Complications can include urinary tract infections, bladder stones, and chronic kidney problems.

Retrograde ejaculation occurs when semen which would be ejaculated via the urethra is redirected to the urinary bladder. Normally, the sphincter of the bladder contracts before ejaculation, sealing the bladder which besides inhibiting the release of urine also prevents a reflux of seminal fluids into the male bladder during ejaculation. The semen is forced to exit via the urethra, the path of least resistance. When the bladder sphincter does not function properly, retrograde ejaculation may occur. It can also be induced deliberately by a male as a primitive form of male birth control or as part of certain alternative medicine practices. The retrograde-ejaculated semen, which goes into the bladder, is excreted with the next urination.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.
Transurethral resection of the prostate is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, it is performed by visualising the prostate through the urethra and removing tissue by electrocautery or sharp dissection. It has been the standard treatment for BPH for many years, but recently alternative, minimally invasive techniques have become available. This procedure is done with spinal or general anaesthetic. A triple lumen catheter is inserted through the urethra to irrigate and drain the bladder after the surgical procedure is complete. Outcome is considered excellent for 80–90% of BPH patients. The procedure carries minimal risk for erectile dysfunction, moderate risk for bleeding, and a large risk for retrograde ejaculation.

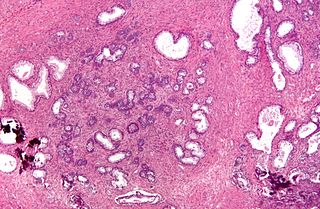
Hyperplasia, or hypergenesis, is an enlargement of an organ or tissue caused by an increase in the amount of organic tissue that results from cell proliferation. It may lead to the gross enlargement of an organ, and the term is sometimes confused with benign neoplasia or benign tumor.

Prostatectomy as a medical term refers to the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

Tamsulosin, sold under the brand name Flomax among others, is a medication used to treat symptomatic benign prostatic hyperplasia (BPH) and chronic prostatitis and to help with the passage of kidney stones. The evidence for benefit with a kidney stone is better when the stone is larger. It is taken by mouth.

Radical perineal prostatectomy is a surgical procedure wherein the entire prostate gland is removed through an incision in the area between the anus and the scrotum (perineum).
Transurethral needle ablation is a technique that uses low energy radio frequency delivered through two needles to ablate excess prostate tissue. A cystoscope/catheter deploys the needles toward the obstructing prostate tissue is inserted into the urethra directly through the penis under local anesthetic before the procedure begins. The energy from the probe heats the abnormal prostate tissue without damaging the urethra. The resulting scar tissue later atrophies, reducing the size of the prostate which in turn reduces the constriction of the urethra. It can be done with a local anesthetic on an outpatient basis. It takes about an hour to perform the procedure. It takes about 30 days for the ablated prostate tissue to resorb.
Saw palmetto extract is an extract of the fruit of the saw palmetto. It is marketed as a treatment for benign prostatic hyperplasia, but there is no clinical evidence that it is effective for this purpose.

A prostatic stent is a stent used to keep open the male urethra and allow the passing of urine in cases of prostatic obstruction and lower urinary tract symptoms (LUTS). Prostatic obstruction is a common condition with a variety of causes. Benign prostatic hyperplasia (BPH) is the most common cause, but obstruction may also occur acutely after treatment for BPH such as transurethral needle ablation of the prostate (TUNA), transurethral resection of the prostate (TURP), transurethral microwave thermotherapy (TUMT), prostate cancer or after radiation therapy.
Lower urinary tract symptoms (LUTS) refer to a group of clinical symptoms involving the bladder, urinary sphincter, urethra and, in men, the prostate. The term is more commonly applied to men—over 40% of older men are afected—but lower urinary tract symptoms also affect women. The condition is also termed prostatism in men, but LUTS is preferred.
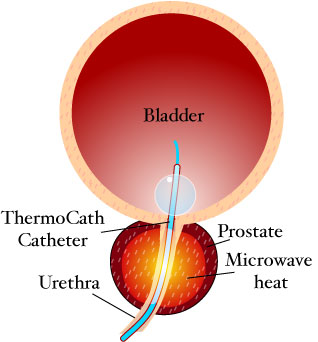
Transurethral microwave thermotherapy (TUMT) is one of a number of effective and safe procedures used in the treatment of lower urinary tract symptoms caused by benign prostatic hyperplasia. It is an alternative treatment to pharmacotherapy such as alpha blockers, transurethral resection of the prostate (TURP), transurethral needle ablation of the prostate, photoselective vaporization of the prostate and prostatic removal or prostatectomy.

High-grade prostatic intraepithelial neoplasia (HGPIN) is an abnormality of prostatic glands and believed to precede the development of prostate adenocarcinoma.

Prostatic artery embolization is a developing non-surgical technique for treatment of benign prostatic hypertrophy (BPH). Although there is increasing research on PAE, use of the technique remains at an incipient stage.

If medical treatment is not effective, surgery may need to be performed for benign prostatic hyperplasia.
Aquablation therapy (AquaBeam) is a surgical procedure for men with lower urinary tract symptoms resulting from benign prostatic hyperplasia (BPH). It is in the early stages of study. It is not categorized as minimally invasive as general anesthesia is required. The procedure was developed by PROCEPT BioRobotics and combines real-time visualization through a cystoscope and a bi-plane ultrasound, while using a high-velocity sterile saline heat-free waterjet and autonomous robotics to remove prostate tissue.
Prostate steam treatment (Rezum), also called water vapor thermal therapy (WVTT), is a minimally invasive surgical procedure for men with lower urinary tract symptoms resulting from prostate enlargement. It uses injections of steam to remove obstructive prostate tissue from the inside of the organ without injuring the prostatic part of the urinary tube.
Prostatic urethral lift is a minimally invasive procedure for the treatment of benign prostatic hyperplasia. This procedure can be done under local anesthesia in an outpatient consultation.
References
- ↑ Christopher R. Chapple; John D. McConnell; Andrea Tubaro (1 August 2000). Benign prostatic hyperplasia: current therapy. Taylor & Francis. pp. 93–. ISBN 978-1-85317-603-6 . Retrieved 14 June 2011.