History
National Cancer Act of 1971
| External videos | |
|---|---|
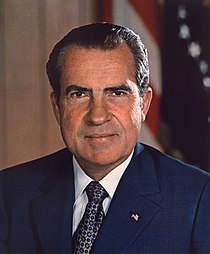 | |
The war on cancer began with the National Cancer Act of 1971, a United States federal law. [9] The act was intended "to amend the Public Health Service Act so as to strengthen the National Cancer Institute in order to more effectively carry out the national effort against cancer". [1] It was signed into law by President Nixon on December 23, 1971. [10]
Health activist and philanthropist Mary Lasker was instrumental in persuading the United States Congress to pass the National Cancer Act. [11] She and her husband Albert Lasker were strong supporters of medical research. They established the Lasker Foundation which awarded people for their research. In the year of 1943, Mary Lasker began changing the American Cancer Society to get more funding for research. Five years later she contributed to getting federal funding for the National Cancer Institute and the National Heart Institute. In 1946 the funding was around $2.8 million and had grown to over $1.4 billion by 1972. In addition to all of these accomplishments, Mary became the president of the Lasker Foundation due to the death of her husband in 1952. Lasker's devotion to medical research and experience in the field eventually contributed to the passing of the National Cancer Act. [12]
The improved funding for cancer research has been quite beneficial over the last 40 years. In 1971, the number of survivors in the U.S. was 3 million and as of 2007 has increased to more than 12 million. [13]
NCI Director's Challenge
In 2003, Andrew von Eschenbach, the director of the National Cancer Institute (who served as FDA Commissioner from 2006 to 2009 and is now a Director at biotechnology company BioTime) issued a challenge "to eliminate the suffering and death from cancer, and to do so by 2015". [14] [15] This was supported by the American Association for Cancer Research in 2005 [16] though some scientists felt this goal was impossible to reach and undermined von Eschenbach's credibility. [17]
John E. Niederhuber, who succeeded Andrew von Eschenbach as NCI director, noted that cancer is a global health crisis, with 12.9 million new cases diagnosed in 2009 worldwide and that by 2030, this number could rise to 27 million including 17 million deaths "unless we take more pressing action". [18]
Harold Varmus, former director of the NIH and director of the NCI from 2010 to 2015, [19] [20] held a town hall meeting in 2010 [21] in which he outlined his priorities for improving the cancer research program, including the following:
- reforming the clinical trials system,
- improving utilization of the NIH clinical center (Mark O. Hatfield Clinical Research Center),
- readjusting the drug approval and regulation processes,
- improving cancer treatment and prevention, and
- formulating new, more specific and science-based questions.
Renewed focus on cancer
Recent years have seen an increased perception of a lack of progress in the war on cancer, and renewed motivation to confront the disease. [5] [22] On July 15, 2008, the United States Senate Committee on Health, Education, Labor, and Pensions convened a panel discussion titled, Cancer: Challenges and Opportunities in the 21st Century. [23] It included interviews with noted cancer survivors such as Arlen Specter, Elizabeth Edwards and Lance Armstrong, who came out of retirement in 2008, returning to competitive cycling "to raise awareness of the global cancer burden". [24]
Livestrong Foundation
The Livestrong Foundation created the Livestrong Global Cancer Campaign to address the burden of cancer worldwide and encourage nations to make commitments to battle the disease and provide better access to care. [25] In April 2009, the foundation announced that the Hashemite Kingdom of Jordan pledged $300 million to fund three important cancer control initiatives – building a cutting-edge cancer treatment and research facility, developing a national cancer control plan and creating an Office of Advocacy and Survivorship. [26] The Livestrong Foundation encourages similar commitments from other nations to combat the disease.
Livestrong Day is an annual event established by the LAF to serve as "a global day of action to raise awareness about the fight against cancer". Individuals from around the world are encouraged to host cancer-oriented events in their local communities and then register their events with the Livestrong website. [27]
21st Century Cancer Access to Life-Saving Early detection, Research and Treatment (ALERT) Act
The US Senate on 26 March 2009 issued a new bill (S. 717), the 21st Century Cancer Access to Life-Saving Early detection, Research and Treatment (ALERT) Act [28] intended to "overhaul the 1971 National Cancer Act." [7] The bill aims to improve patient access to prevention and early detection by:
- providing funding for research in early detection,
- supplying grants for screening and referrals for treatment, and
- increasing access to clinical trials and information.
Obama-Biden Plan to Combat Cancer
During their 2008 U.S. presidential campaign then Senators Barack Obama and Joe Biden published a plan to combat cancer that entailed doubling "federal funding for cancer research within 5 years, focusing on NIH and NCI" as well as working "with Congress to increase funding for the Food and Drug Administration." [29] [30] Their plan would provide additional funding for:
- research on rare cancers and those without effective treatment options,
- the study of health disparities and evaluation of possible interventions,
- and efforts to better understand genetic factors that can impact cancer onset and outcomes.
President Obama's 2009 economic stimulus package includes $10 billion for the NIH, which funds much of the cancer research in the U.S., and he has pledged to increase federal funding for cancer research by a third for the next two years as part of a drive to find "a cure for cancer in our time". [31] [32] In a message published in the July 2009 issue of Harper's Bazaar, President Obama described his mother's battle with ovarian cancer and, noting the additional funding his administration has slated for cancer research, stated: "Now is the time to commit ourselves to waging a war against cancer as aggressive as the war cancer wages against us." [33] On 30 September 2009, Obama announced that $1 billion of a $5 billion medical research spending plan would be earmarked for research into the genetic causes of cancer and targeted cancer treatments. [34]
Cancer-related federal spending of money from the 2009 Recovery Act can be tracked online. [35]
World Cancer Campaign
The International Union Against Cancer (UICC) has organized a World Cancer campaign in 2009 with the theme, "I love my healthy active childhood," to promote healthy habits in children and thereby reduce their lifestyle-based cancer risk as adults. [36] The World Health Organization is also promoting this campaign [37] and joins with the UICC in annually promoting World Cancer Day on 4 February. [38]
United States' 2022 Moonshot 2.0
Joe Biden announced Moonshot 2.0, a new front in the war on cancer on 4 February 2022 as part of World Cancer Day. [39] [40] As part of the Moonshot 2.0, the Biden administration set a goal of reducing cancer death rate by at least 50 percent over the next 25 years, and improving the experience of living with and surviving cancer. The new effort will signal a "reignition" of the "cancer moonshot" Biden began as vice president under Barack Obama. Moonshot 2.0 was reported to be deeply imbued with personal grief, since the president's son Beau had died the year before from brain cancer. [41]
Biden's new plan calls for a "cancer Cabinet", as well as a new federal agency for high-level research for which his administration is seeking $6.5 billion in seed funding. The president named Danielle Carnival, a neuroscientist who worked on the 2016 cancer initiative, to oversee the moonshot's second version. [42] Moonshot 2.0 would continue work from 2016, involving fostering public-private partnerships, including with biomedical giants, community organizations and academic institutions.
The administration noted that the pandemic showed that researchers collaborating across countries and regulatory barriers could work to produce vaccines whose safety and efficacy are widely regarded as "a marvel of science". On the same day that Moonshot 2.0 was launched, the United Kingdom, a key ally and important research partner, launched their 2022 National War on Cancer .
Specifically, the White House announced new goals outlining:
- Working together over the next 25 years, to will cut today's age-adjusted death rate from cancer by at least 50 percent.
- To improve the experience of people and their families living with and surviving cancer.
The Moonshot 2.0 statement detailed actions that the White House stated would drive us toward ending cancer as we know it today
- To diagnose cancer sooner. Noting "we can also greatly expand the cancers we can screen for. Five years ago, detecting many cancers at once through blood tests was a dream. Now new technologies and rigorous clinical trials could put this within our reach"
- To prevent cancer
- To address inequities. Noting a plan to ensure that every community in America – rural, urban, Tribal, and everywhere else – has access to cutting-edge cancer diagnostics, therapeutics, and clinical trials.
- To target the right treatments to the right patients
- To speed progress against the most deadly and rare cancers, including childhood cancers
- To support patients, caregivers, and survivors
- To learn from all patients
- Re-establish White House Leadership with a White House Cancer Moonshot coordinator in the Executive Office of the President, to demonstrate the President and First Lady's personal commitment to making progress and to leverage the whole-of-government approach and national response that the challenge of cancer demands. And additionally form a Cancer Cabinet, and host a White House Cancer Moonshot Summit.
- Issue a Call to Action on Cancer Screening and Early Detection.
United Kingdom's 2022 National War on Cancer
The United Kingdom initiated a 10-year National war on cancer on World Cancer Day on 4 February 2022. [43] This was on the same day as United States' 2022 Moonshot 2.0 initiative calling for increasing collaboration for a new front in the war on cancer across countries. It was launched by the Health and Social Care Secretary Sajid Javid at the Francis Crick institute in London. Started in the shadow of the third coronavirus wave in the United Kingdom, Sajid Javid promised the National War on Cancer will "make the UK's cancer care system "the best in Europe"", [44] and "show how we are learning the lessons from the pandemic, and apply them to improving cancer services over the next decade".
A set of six new and strengthened priorities were made public including:-
- Increasing the number of people diagnosed at an early stage where treatment can prove much more effective
- Intensifying research on new early diagnostic tools to catch cancer at an earlier stage. A key strategy of the National War on Cancer was building on the latest scientific advances and partnering with the country's technology pioneers. The United Kingdom's NHS-Galleri trial is evaluating a new test that looks for distinct markers in blood to identify cancer risk and was listed as a key example of how technology can transform the way cancer is detected. The test is being trialled across England, with thousands of people already recruited. The UK government wants similar technologies to help form new partnerships and give their National Health Service early, cost effective access to new diagnostics.
- Intensifying research on mRNA vaccines and therapeutics for cancer – this will be achieved through the UK's global leadership and supporting industry to develop new cancer treatments by combining expertise in cancer immunotherapy treatment and the vaccine capabilities developed throughout the pandemic
- Improving prevention of cancer through tackling the big known risk factors such as smoking
- Boosting the cancer workforce
- Tackling disparities and inequalities, including in cancer diagnosis times and ensuring recovery from the pandemic is delivered in a fair way – for instance, the "Help Us Help You" cancer awareness campaign will be directed towards people from more deprived groups and ethnic minorities










