A transient ischemic attack (TIA), commonly known as a mini-stroke, is a minor stroke whose noticeable symptoms usually end in less than an hour. TIA causes the same symptoms associated with strokes, such as weakness or numbness on one side of the body, sudden dimming or loss of vision, difficulty speaking or understanding language, slurred speech, or confusion.

An atheroma, or atheromatous plaque, is an abnormal accumulation of material in the inner layer of an arterial wall.
Intravascular ultrasound (IVUS) or intravascular echocardiography is a medical imaging methodology using a specially designed catheter with a miniaturized ultrasound probe attached to the distal end of the catheter. The proximal end of the catheter is attached to computerized ultrasound equipment. It allows the application of ultrasound technology, such as piezoelectric transducer or CMUT, to see from inside blood vessels out through the surrounding blood column, visualizing the endothelium of blood vessels.
A vulnerable plaque is a kind of atheromatous plaque – a collection of white blood cells and lipids in the wall of an artery – that is particularly unstable and prone to produce sudden major problems such as a heart attack or stroke.

Cerebral angiography is a form of angiography which provides images of blood vessels in and around the brain, thereby allowing detection of abnormalities such as arteriovenous malformations and aneurysms. It was pioneered in 1927 by the Portuguese neurologist Egas Moniz at the University of Lisbon, who also helped develop thorotrast for use in the procedure.

Renal artery stenosis (RAS) is the narrowing of one or both of the renal arteries, most often caused by atherosclerosis or fibromuscular dysplasia. This narrowing of the renal artery can impede blood flow to the target kidney, resulting in renovascular hypertension – a secondary type of high blood pressure. Possible complications of renal artery stenosis are chronic kidney disease and coronary artery disease.

Carotid endarterectomy is a surgical procedure used to reduce the risk of stroke from carotid artery stenosis. In endarterectomy, the surgeon opens the artery and removes the plaque. The plaque forms and thickens the inner layer of the artery, or intima, hence the name of the procedure which simply means removal of part of the internal layers of the artery.

Carotid artery stenosis is a narrowing or constriction of any part of the carotid arteries, usually caused by atherosclerosis.

Magnetic resonance angiography (MRA) is a group of techniques based on magnetic resonance imaging (MRI) to image blood vessels. Magnetic resonance angiography is used to generate images of arteries in order to evaluate them for stenosis, occlusions, aneurysms or other abnormalities. MRA is often used to evaluate the arteries of the neck and brain, the thoracic and abdominal aorta, the renal arteries, and the legs.

Transcranial Doppler (TCD) and transcranial color Doppler (TCCD) are types of Doppler ultrasonography that measure the velocity of blood flow through the brain's blood vessels by measuring the echoes of ultrasound waves moving transcranially. These modes of medical imaging conduct a spectral analysis of the acoustic signals they receive and can therefore be classified as methods of active acoustocerebrography. They are used as tests to help diagnose emboli, stenosis, vasospasm from a subarachnoid hemorrhage, and other problems. These relatively quick and inexpensive tests are growing in popularity. The tests are effective for detecting sickle cell disease, ischemic cerebrovascular disease, subarachnoid hemorrhage, arteriovenous malformations, and cerebral circulatory arrest. The tests are possibly useful for perioperative monitoring and meningeal infection. The equipment used for these tests is becoming increasingly portable, making it possible for a clinician to travel to a hospital, to a doctor's office, or to a nursing home for both inpatient and outpatient studies. The tests are often used in conjunction with other tests such as MRI, MRA, carotid duplex ultrasound and CT scans. The tests are also used for research in cognitive neuroscience.

Digital subtraction angiography (DSA) is a fluoroscopy technique used in interventional radiology to clearly visualize blood vessels in a bony or dense soft tissue environment. Images are produced using contrast medium by subtracting a "pre-contrast image" or mask from subsequent images, once the contrast medium has been introduced into a structure. Hence the term "digital subtraction angiography. Subtraction angiography was first described in 1935 and in English sources in 1962 as a manual technique. Digital technology made DSA practical starting in the 1970s.

A watershed stroke is defined as a brain ischemia that is localized to the vulnerable border zones between the tissues supplied by the anterior, posterior and middle cerebral arteries. The actual blood stream blockage/restriction site can be located far away from the infarcts. Watershed locations are those border-zone regions in the brain supplied by the major cerebral arteries where blood supply is decreased. Watershed strokes are a concern because they comprise approximately 10% of all ischemic stroke cases. The watershed zones themselves are particularly susceptible to infarction from global ischemia as the distal nature of the vasculature predisposes these areas to be most sensitive to profound hypoperfusion.
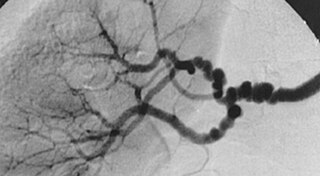
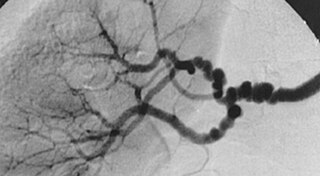
Fibromuscular dysplasia (FMD) is a non-atherosclerotic, non-inflammatory disease of the blood vessels that causes abnormal growth within the wall of an artery. FMD has been found in nearly every arterial bed in the body, although the most commonly affected are the renal and carotid arteries.

Subclavian steal syndrome (SSS), also called subclavian steal steno-occlusive disease, is a constellation of signs and symptoms that arise from retrograde (reversed) blood flow in the vertebral artery or the internal thoracic artery, due to a proximal stenosis (narrowing) and/or occlusion of the subclavian artery. This flow reversal is called the subclavian steal or subclavian steal phenomenon, regardless of signs/symptoms being present. The arm may be supplied by blood flowing in a retrograde direction down the vertebral artery at the expense of the vertebrobasilar circulation. It is more severe than typical vertebrobasilar insufficiency.

Computed tomography angiography is a computed tomography technique used for angiography—the visualization of arteries and veins—throughout the human body. Using contrast injected into the blood vessels, images are created to look for blockages, aneurysms, dissections, and stenosis. CTA can be used to visualize the vessels of the heart, the aorta and other large blood vessels, the lungs, the kidneys, the head and neck, and the arms and legs. CTA can also be used to localise arterial or venous bleed of the gastrointestinal system.
John David Spence is a Canadian medical doctor, medical researcher and Professor Emeritus at the University of Western Ontario. He is affiliated with the University of Western Ontario and the Robarts Research Institute, one of Canada's leading medical research organizations. Before his retirement from clinical practice in July 2022, he was also affiliated with the London Health Sciences Centre's University Hospital. He is a recognized expert in stroke prevention and stroke prevention research, with more than 600 peer-reviewed publications since 1970. He delivered more than 600 lectures on stroke prevention in 42 countries. In 2015, he received the Research Excellence Award from the Canadian Society for Atherosclerosis, Thrombosis and Vascular Biology. In 2019, he was appointed a Member of the Order of Canada, and in 2020 he received the William Feinberg Award from the American Heart Association for excellence in clinical stroke research.
Tissue Doppler echocardiography (TDE) is a medical ultrasound technology, specifically a form of echocardiography that measures the velocity of the heart muscle (myocardium) through the phases of one or more heartbeats by the Doppler effect of the reflected ultrasound. The technique is the same as for flow Doppler echocardiography measuring flow velocities. Tissue signals, however, have higher amplitude and lower velocities, and the signals are extracted by using different filter and gain settings. The terms tissue Doppler imaging (TDI) and tissue velocity imaging (TVI) are usually synonymous with TDE because echocardiography is the main use of tissue Doppler.

Doppler ultrasonography is medical ultrasonography that employs the Doppler effect to perform imaging of the movement of tissues and body fluids, and their relative velocity to the probe. By calculating the frequency shift of a particular sample volume, for example, flow in an artery or a jet of blood flow over a heart valve, its speed and direction can be determined and visualized.
Penile ulltrasonography is medical ultrasonography of the penis. Ultrasound is an excellent method for the study of the penis, such as indicated in trauma, priapism, erectile dysfunction or suspected Peyronie's disease.

Arterial occlusion is a condition involving partial or complete blockage of blood flow through an artery. Arteries are blood vessels that carry oxygenated blood to body tissues. An occlusion of arteries disrupts oxygen and blood supply to tissues, leading to ischemia. Depending on the extent of ischemia, symptoms of arterial occlusion range from simple soreness and pain that can be relieved with rest, to a lack of sensation or paralysis that could require amputation.