Related Research Articles
Cost-effectiveness analysis (CEA) is a form of economic analysis that compares the relative costs and outcomes (effects) of different courses of action. Cost-effectiveness analysis is distinct from cost–benefit analysis, which assigns a monetary value to the measure of effect. Cost-effectiveness analysis is often used in the field of health services, where it may be inappropriate to monetize health effect. Typically the CEA is expressed in terms of a ratio where the denominator is a gain in health from a measure and the numerator is the cost associated with the health gain. The most commonly used outcome measure is quality-adjusted life years (QALY).
The incremental cost-effectiveness ratio (ICER) is a statistic used in cost-effectiveness analysis to summarise the cost-effectiveness of a health care intervention. It is defined by the difference in cost between two possible interventions, divided by the difference in their effect. It represents the average incremental cost associated with 1 additional unit of the measure of effect. The ICER can be estimated as:
Cost–benefit analysis (CBA), sometimes also called benefit–cost analysis, is a systematic approach to estimating the strengths and weaknesses of alternatives. It is used to determine options which provide the best approach to achieving benefits while preserving savings in, for example, transactions, activities, and functional business requirements. A CBA may be used to compare completed or potential courses of action, and to estimate or evaluate the value against the cost of a decision, project, or policy. It is commonly used to evaluate business or policy decisions, commercial transactions, and project investments. For example, the U.S. Securities and Exchange Commission must conduct cost-benefit analyses before instituting regulations or deregulations.

Preventive healthcare, or prophylaxis, is the application of healthcare measures to prevent diseases. Disease and disability are affected by environmental factors, genetic predisposition, disease agents, and lifestyle choices, and are dynamic processes that begin before individuals realize they are affected. Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.

The quality-adjusted life year (QALY) is a generic measure of disease burden, including both the quality and the quantity of life lived. It is used in economic evaluation to assess the value of medical interventions. One QALY equates to one year in perfect health. QALY scores range from 1 to 0 (dead). QALYs can be used to inform health insurance coverage determinations, treatment decisions, to evaluate programs, and to set priorities for future programs.
Disease management is defined as "a system of coordinated healthcare interventions and communications for populations with conditions in which patient self-care efforts are significant."
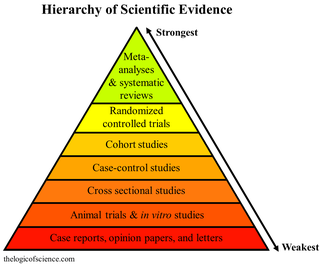
A systematic review is a scholarly synthesis of the evidence on a clearly presented topic using critical methods to identify, define and assess research on the topic. A systematic review extracts and interprets data from published studies on the topic, then analyzes, describes, critically appraises and summarizes interpretations into a refined evidence-based conclusion. For example, a systematic review of randomized controlled trials is a way of summarizing and implementing evidence-based medicine.

Extracorporeal shockwave therapy (ESWT) is a non-invasive, out-patient alternative to surgery for those with many joint and tendon disorders. ESWT sends acoustic shock waves into bone or soft tissue, in effect reinjuring the area on a cellular level and breaking up the scarring that has penetrated tendons and ligaments. The controlled reinjuring of tissue allows the body to regenerate blood vessels and bone cells. The resulting revascularization leads to faster healing and often a return to pre-injury activity levels. ESWT is mostly used for kidney stones removal, in physical therapy and orthopedics.

Vaccine efficacy or vaccine effectiveness is the percentage reduction of disease cases in a vaccinated group of people compared to an unvaccinated group. For example, a vaccine efficacy or effectiveness of 80% indicates an 80% decrease in the number of disease cases among a group of vaccinated people compared to a group in which nobody was vaccinated. When a study is carried out using the most favorable, ideal or perfectly controlled conditions, such as those in a clinical trial, the term vaccine efficacy is used. On the other hand, when a study is carried out to show how well a vaccine works when they are used in a bigger, typical population under less-than-perfectly controlled conditions, the term vaccine effectiveness is used.
Cardiac rehabilitation (CR) is defined by the World Health Organization (WHO) as "the sum of activity and interventions required to ensure the best possible physical, mental, and social conditions so that patients with chronic or post-acute cardiovascular disease may, by their own efforts, preserve or resume their proper place in society and lead an active life". CR is a comprehensive model of care delivering established core components, including structured exercise, patient education, psychosocial counselling, risk factor reduction and behaviour modification, with a goal of optimizing patient's quality of life and reducing the risk of future heart problems.
Early intervention in psychosis is a clinical approach to those experiencing symptoms of psychosis for the first time. It forms part of a new prevention paradigm for psychiatry and is leading to reform of mental health services, especially in the United Kingdom and Australia.
Comparative effectiveness research (CER) is the direct comparison of existing health care interventions to determine which work best for which patients and which pose the greatest benefits and harms. The core question of comparative effectiveness research is which treatment works best, for whom, and under what circumstances. Engaging various stakeholders in this process, while difficult, makes research more applicable through providing information that improves patient decision making.

Targeted intra-operative radiotherapy, also known as targeted IORT, is a technique of giving radiotherapy to the tissues surrounding a cancer after its surgical removal, a form of intraoperative radiation therapy. The technique was designed in 1998 at the University College London.

Remote patient monitoring (RPM) is a technology to enable monitoring of patients outside of conventional clinical settings, such as in the home or in a remote area, which may increase access to care and decrease healthcare delivery costs. RPM involves the constant remote care of patients by their physicians, often to track physical symptoms, chronic conditions, or post-hospitalization rehab.

Mass deworming, is one of the preventive chemotherapy tools, used to treat large numbers of people, particularly children, for worm infections notably soil-transmitted helminthiasis, and schistosomiasis in areas with a high prevalence of these conditions. It involves treating everyone – often all children who attend schools, using existing infrastructure to save money – rather than testing first and then only treating selectively. Serious side effects have not been reported when administering the medication to those without worms, and testing for the infection is many times more expensive than treating it. Therefore, for the same amount of money, mass deworming can treat more people more cost-effectively than selective deworming. Mass deworming is one example of mass drug administration.
In global health, priority-setting is a term used for the process and strategy of deciding which health interventions to carry out. Priority-setting can be conducted at the disease level, the overall strategy level, research level, or other levels.
WHO-CHOICE is an initiative started by the World Health Organization in 1998 to help countries choose their healthcare priorities. It is an example of priority-setting in global health. It was one of the earliest projects to perform sectoral cost-effectiveness analyses on a global scale. Findings from WHO-CHOICE have shaped the World Health Report of 2002, been published in the British Medical Journal in 2012, and been cited by charity evaluators and academics alongside DCP2 and the Copenhagen Consensus.
Prostate steam treatment (Rezum), also called water vapor thermal therapy (WVTT), is a minimally invasive surgical procedure for men with lower urinary tract symptoms resulting from prostate enlargement. It uses injections of steam to remove obstructive prostate tissue from the inside of the organ without injuring the prostatic part of the urinary tube.
Value-based health care (VBHC) is a framework for restructuring health care systems with the overarching goal of value for patients, with value defined as health outcomes per unit of costs. The concept was introduced in 2006 by Michael Porter and Elizabeth Olmsted Teisberg, though implementation efforts on aspects of value-based care began long before then in the 1990s. With patient value as the overarching goal, VBHC emphasis systematic measurement of outcomes and costs, restructuring provider organizations, and transitioning toward bundled payments. Within this framework, cost reduction alone is not seen as proper strategy for healthcare systems: health outcomes have to improve to enhance value. Although value-based health care is seen as a priority in many health systems worldwide, a global assessment in 2016 found many countries are only beginning to align their health systems with VBHC-principles. Additionally, several studies report incoherent implementation efforts, and there seem to be various interpretations of VBHC, both within and across countries.

Etheldreda Nakimuli-Mpungu is a professor, researcher, epidemiologist and psychiatrist at the Department of Psychiatry in the Faculty of Medicine, Makerere University in Uganda. Her research is particularly focused on supportive group psychotherapy as a first-line treatment for depression in people with HIV. She is one of only five recipients of the Elsevier Foundation Award for Early Career Women Scientists in the Developing World in Biological Sciences, as well as listed at one of the BBC's 100 Women in 2020.
References
- ↑ Asaria, M; Griffin, S; Cookson, R; Whyte, S; Tappenden, P (June 2015). "Distributional cost-effectiveness analysis of health care programmes--a methodological case study of the UK Bowel Cancer Screening Programme" (PDF). Health Economics. 24 (6): 742–54. doi: 10.1002/hec.3058 . PMID 24798212.
- ↑ Asaria, M; Griffin, S; Cookson, R (January 2016). "Distributional Cost-Effectiveness Analysis: A Tutorial". Medical Decision Making. 36 (1): 8–19. doi:10.1177/0272989x15583266. PMC 4853814 . PMID 25908564.
- ↑ Verguet, Stéphane; Kim, Jane J.; Jamison, Dean T. (2016). "Extended Cost-Effectiveness Analysis for Health Policy Assessment: A Tutorial". Pharmacoeconomics. 34 (9): 913–923. doi:10.1007/s40273-016-0414-z. ISSN 1170-7690. PMC 4980400 . PMID 27374172.