Acupressure is an alternative medicine technique often used in conjunction with acupuncture or reflexology. It is based on the concept of life energy, which flows through "meridians" in the body. In treatment, physical pressure is applied to acupuncture points, or ashi trigger points, with the aim of clearing blockages in these meridians. Pressure may be applied by hand, by elbow, or with various devices.

Transcranial magnetic stimulation (TMS) is a noninvasive form of brain stimulation in which a changing magnetic field is used to induce an electric current at a specific area of the brain through electromagnetic induction. An electric pulse generator, or stimulator, is connected to a magnetic coil connected to the scalp. The stimulator generates a changing electric current within the coil which creates a varying magnetic field, inducing a current within a region in the brain itself.
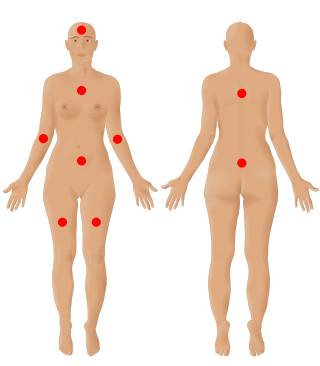
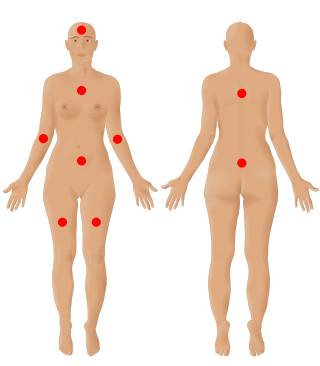
Fibromyalgia is a medical condition which causes chronic widespread pain, accompanied by fatigue, waking unrefreshed and cognitive symptoms. Other symptoms include headaches, lower abdominal pain or cramps, and depression. People with fibromyalgia can also experience insomnia and a general hypersensitivity.

Cranial electrotherapy stimulation (CES) is a form of neurostimulation that delivers a small, pulsed, alternating current via electrodes on the head. CES is used with the intention of treating a variety of conditions such as anxiety, depression and insomnia. CES has been suggested as a possible treatment for headaches, fibromyalgia, smoking cessation, and opiate withdrawal, but there is little evidence of effectiveness for many of these conditions and the evidence for use in acute depression is not sufficient to justify it.
Diabetic neuropathy is various types of nerve damage associated with diabetes mellitus. Symptoms depend on the site of nerve damage and can include motor changes such as weakness; sensory symptoms such as numbness, tingling, or pain; or autonomic changes such as urinary symptoms. These changes are thought to result from a microvascular injury involving small blood vessels that supply nerves. Relatively common conditions which may be associated with diabetic neuropathy include distal symmetric polyneuropathy; third, fourth, or sixth cranial nerve palsy; mononeuropathy; mononeuropathy multiplex; diabetic amyotrophy; and autonomic neuropathy.

Peripheral neuropathy, often shortened to neuropathy, is a general term describing damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

Low back pain or lumbago is a common disorder involving the muscles, nerves, and bones of the back, in between the lower edge of the ribs and the lower fold of the buttocks. Pain can vary from a dull constant ache to a sudden sharp feeling. Low back pain may be classified by duration as acute, sub-chronic, or chronic. The condition may be further classified by the underlying cause as either mechanical, non-mechanical, or referred pain. The symptoms of low back pain usually improve within a few weeks from the time they start, with 40–90% of people recovered by six weeks.

A transcutaneous electrical nerve stimulation is a device that produces mild electric current to stimulate the nerves for therapeutic purposes. TENS, by definition, covers the complete range of transcutaneously applied currents used for nerve excitation, but the term is often used with a more restrictive intent—namely, to describe the kind of pulses produced by portable stimulators used to reduce pain. The unit is usually connected to the skin using two or more electrodes which are typically conductive gel pads. A typical battery-operated TENS unit is able to modulate pulse width, frequency, and intensity. Generally, TENS is applied at high frequency (>50 Hz) with an intensity below motor contraction or low frequency (<10 Hz) with an intensity that produces motor contraction. More recently, many TENS units use a mixed frequency mode which alleviates tolerance to repeated use. Intensity of stimulation should be strong but comfortable with greater intensities, regardless of frequency, producing the greatest analgesia. While the use of TENS has proved effective in clinical studies, there is controversy over which conditions the device should be used to treat.

Pressure ulcers, also known as pressure sores, bed sores or pressure injuries, are localised damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of usually long-term pressure, or pressure in combination with shear or friction. The most common sites are the skin overlying the sacrum, coccyx, heels, and hips, though other sites can be affected, such as the elbows, knees, ankles, back of shoulders, or the back of the cranium.
The primary goals of stroke management are to reduce brain injury and promote maximum patient recovery. Rapid detection and appropriate emergency medical care are essential for optimizing health outcomes. When available, patients are admitted to an acute stroke unit for treatment. These units specialize in providing medical and surgical care aimed at stabilizing the patient's medical status. Standardized assessments are also performed to aid in the development of an appropriate care plan. Current research suggests that stroke units may be effective in reducing in-hospital fatality rates and the length of hospital stays.

Venous ulcer is defined by the American Venous Forum as "a full-thickness defect of skin, most frequently in the ankle region, that fails to heal spontaneously and is sustained by chronic venous disease, based on venous duplex ultrasound testing." Venous ulcers are wounds that are thought to occur due to improper functioning of venous valves, usually of the legs. They are an important cause of chronic wounds, affecting 1% of the population. Venous ulcers develop mostly along the medial distal leg, and can be painful with negative effects on quality of life.
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease that affects the central nervous system (CNS). Several therapies for it exist, although there is no known cure.

Extracorporeal shockwave therapy (ESWT) is a treatment using powerful acoustic pulses which is mostly used to treat kidney stones and in physical therapy and orthopedics.
Therapeutic ultrasound refers generally to any type of ultrasonic procedure that uses ultrasound for therapeutic benefit. Physiotherapeutic ultrasound was introduced into clinical practice in the 1950s, with lithotripsy introduced in the 1980s. Others are at various stages in transitioning from research to clinical use: HIFU, targeted ultrasound drug delivery, trans-dermal ultrasound drug delivery, ultrasound hemostasis, cancer therapy, and ultrasound assisted thrombolysis It may use focused ultrasound or unfocused ultrasound.

Neck pain, also known as cervicalgia, is a common problem, with two-thirds of the population having neck pain at some point in their lives.

Patellofemoral pain syndrome is knee pain as a result of problems between the kneecap and the femur. The pain is generally in the front of the knee and comes on gradually. Pain may worsen with sitting, excessive use, or climbing and descending stairs.

Radionics—also called electromagnetic therapy (EMT) and the Abrams Method—is a form of alternative medicine that claims that disease can be diagnosed and treated by applying electromagnetic radiation (EMR), such as radio waves, to the body from an electrically powered device. It is similar to magnet therapy, which also applies EMR to the body but uses a magnet that generates a static electromagnetic field.

Low-level laser therapy (LLLT), cold laser therapy, photobiomodulation (PBM) or red light therapy is a form of medicine that applies low-level (low-power) lasers or light-emitting diodes (LEDs) to the surface of the body. Whereas high-power lasers are used in laser medicine to cut or destroy tissue, it is claimed that application of low-power lasers relieves pain or stimulates and enhances cell function. The effects appear to be limited to a specified set of wavelengths and new research has demonstrated effectiveness at myopia control. Several such devices are cleared by the United States Food and Drug Administration (FDA), and research shows potential for treating a range of medical problems including rheumatoid arthritis and oral mucositis.

Pulsed electromagnetic field therapy, also known as low field magnetic stimulation (LFMS) is the use of electromagnetic fields in an attempt to heal non-union fractures and depression. By 2007 the FDA had cleared several such stimulation devices.

Diabetic foot ulcer is a breakdown of the skin and sometimes deeper tissues of the foot that leads to sore formation. It may occur due to a variety of mechanisms. It is thought to occur due to abnormal pressure or mechanical stress chronically applied to the foot, usually with concomitant predisposing conditions such as peripheral sensory neuropathy, peripheral motor neuropathy, autonomic neuropathy or peripheral arterial disease. It is a major complication of diabetes mellitus, and it is a type of diabetic foot disease. Secondary complications to the ulcer, such as infection of the skin or subcutaneous tissue, bone infection, gangrene or sepsis are possible, often leading to amputation.