A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.

Social services are a range of public services intended to provide support and assistance towards particular groups, which commonly include the disadvantaged. They may be provided by individuals, private and independent organisations, or administered by a government agency. Social services are connected with the concept of welfare and the welfare state, as countries with large welfare programs often provide a wide range of social services. Social services are employed to address the wide range of needs of a society. Prior to industrialisation, the provision of social services was largely confined to private organisations and charities, with the extent of its coverage also limited. Social services are now generally regarded globally as a 'necessary function' of society and a mechanism through which governments may address societal issues.

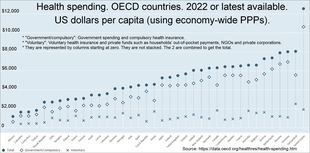
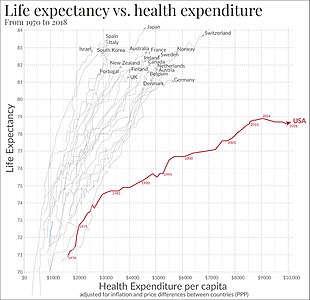
Health economics is a branch of economics concerned with issues related to efficiency, effectiveness, value and behavior in the production and consumption of health and healthcare. Health economics is important in determining how to improve health outcomes and lifestyle patterns through interactions between individuals, healthcare providers and clinical settings. In broad terms, health economists study the functioning of healthcare systems and health-affecting behaviors such as smoking, diabetes, and obesity.

Universal health care is a health care system in which all residents of a particular country or region are assured access to health care. It is generally organized around providing either all residents or only those who cannot afford on their own, with either health services or the means to acquire them, with the end goal of improving health outcomes.
A vaccination policy is a health policy adopted in order to prevent the spread of infectious disease. These policies are generally put into place by State or local governments, but may also be set by private facilities, such as workplaces or schools. Many policies have been developed and implemented since vaccines were first made widely available.

Health may refer to "a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity.", according to the World Health Organization (WHO). 78.7 was the average life expectancy for individuals at birth in 2017. The highest cause of death for United States citizens is heart disease. Infectious diseases such as sexually transmitted diseases impact the health of approximately 19 million yearly. The two most commonly reported infectious diseases include chlamydia and gonorrhea. The United States is currently challenged by the COVID-19 pandemic, and is 19th in the world in COVID-19 vaccination rates. All 50 states in the U.S. require immunizations for children in order to enroll in public school, but various exemptions are available by state. Immunizations are often compulsory for military enlistment in the United States.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, specific healthcare precincts are responsible for providing healthcare to their residents as of 2023.
Healthcare in Georgia is provided by a universal health care system under which the state funds medical treatment in a mainly privatized system of medical facilities. In 2013, the enactment of a universal health care program triggered universal coverage of government-sponsored medical care of the population and improving access to health care services. Responsibility for purchasing publicly financed health services lies with the Social Service Agency (SSA).

Healthcare in Denmark is largely provided by the local governments of the five regions, with coordination and regulation by central government, while nursing homes, home care, and school health services are the responsibility of the 98 municipalities. Some specialised hospital services are managed centrally.
Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance.
Croatia has a universal health care system, whose roots can be traced back to the Hungarian-Croatian Parliament Act of 1891, providing a form of mandatory insurance of all factory workers and craftsmen. The population is covered by a basic health insurance plan provided by statute and optional insurance and administered by the Croatian Health Insurance Fund. In 2012, annual compulsory healthcare related expenditures reached 21.0 billion kuna.
Examples of health care systems of the world, sorted by continent, are as follows.
According to the Constitution of Albania, citizens are entitled to healthcare. The healthcare system in Albania is primarily public. The public system is made up of three tiers: primary care, secondary care, and tertiary care. Primary healthcare covers basic health needs. Secondary healthcare is needed when seeing a specialist after being referred to by a general doctor. Tertiary healthcare funds highly specialized medical care that is needed over a long duration of time. There are over 400 public clinics that offer both primary and secondary healthcare services, along with over 40 public hospitals that offer tertiary healthcare services.

As of 2019 Lithuanian life expectancy at birth was 76.0 and the infant mortality rate was 2.99 per 1,000 births. This is below the EU and OECD average.

New Zealand is a high income country, and this is reflected in the overall good health status of the population. However like other wealthy countries, New Zealand suffers from high rates of obesity and heart disease.
Healthcare in New York City describe the health care services available in New York City, the largest US city with a population of over eight million. In 2020 approximately 50,000 physicians were working in the city.
Montenegro is a country with an area of 13,812 square kilometres and a population of 620,029, according to the 2011 census. The country is bordered by Croatia, the Adriatic Sea, Bosnia, Herzegovina, Serbia, Kosovo and Albania. The most common health issues faced are non-communicable diseases accounting for 95% of all deaths. This is followed by 4% of mortality due to injury, and 1% due to communicable, maternal, perinatal and nutritional conditions. Other health areas of interest are alcohol consumption, which is the most prevalent disease of addiction within Montenegro and smoking. Montenegro has one of the highest tobacco usage rates across Europe. Life expectancy for men is 74 years, and life expectancy for women is 79.
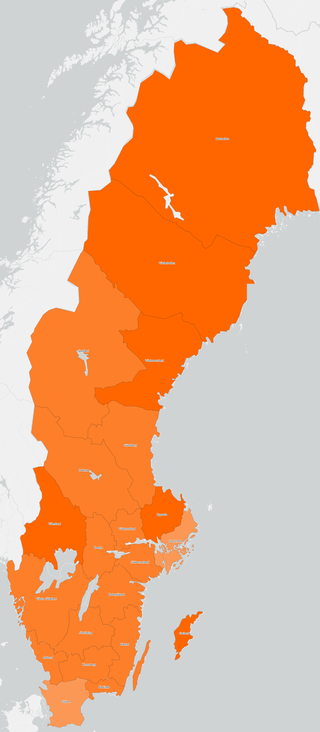
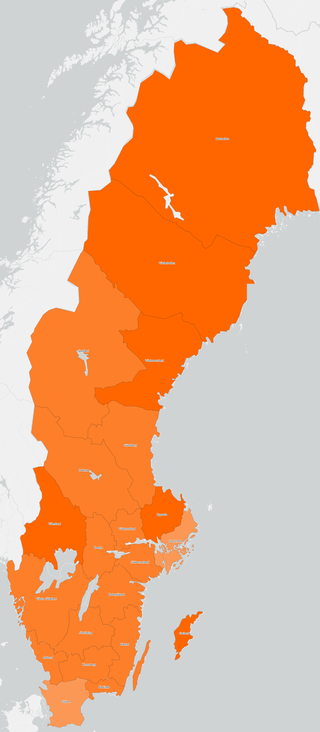
Vaccination against COVID-19 in Sweden started on 27 December 2020 after the approval of the Pfizer–BioNTech vaccine by the European Commission. In Sweden, the Public Health Agency has been commissioned by the government to create a vaccination plan. Sveriges riksbank, the central bank of Sweden, predicts that efficient vaccination against COVID-19 has macroeconomic benefits. As of 20 April 2022, 87.1% of people in Sweden have received at least one dose, with a total of 21,491,717 doses administered. At least one vaccine has been approved for all age groups 12 and older. Children younger than 12 in high risk groups can also be vaccinated.
Vaccination against COVID-19 in Portugal started on 27 December 2020.