NHS Wales is the publicly-funded healthcare system in Wales, and one of the four systems which make up the National Health Service in the United Kingdom.

NHS Scotland, sometimes styled NHSScotland, is the publicly–funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.
Health and Social Care (HSC) is the publicly funded healthcare system in Northern Ireland. Although having been created separately to the National Health Service (NHS), it is nonetheless considered a part of the overall national health service in the United Kingdom. The Northern Ireland Executive through its Department of Health is responsible for its funding, while the Public Health Agency is the executive agency responsible for the provision of public health and social care services across Northern Ireland. It is free of charge to all citizens of Northern Ireland and the rest of the United Kingdom.

Emergency medical services in the United Kingdom provide emergency care to people with acute illness or injury and are predominantly provided free at the point of use by the four National Health Services (NHS) of England, Scotland, Wales, and Northern Ireland. Emergency care including ambulance and emergency department treatment is only free to UK residents and a charge may be made to those not entitled to free NHS care.
National Health Service ambulance services provide free at the point of use emergency medical care to any person requiring treatment, regardless of immigration or visitor status, within the United Kingdom. These services are provided by National Health Services of England, Scotland, Wales and Northern Ireland. The current system comprises 14 NHS organisations: 11 ambulance services trusts cover the separate regions of England and; individual nationwide services cover Scotland, Wales and Northern Ireland respectively.
Imperial College Healthcare NHS Trust is an NHS trust based in London, England. It is one of the largest NHS trusts in England and together with Imperial College London forms an academic health science centre.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use for most people. The NHS also conducts research through the National Institute for Health and Care Research (NIHR).
Healthcare in England is mainly provided by the National Health Service (NHS), a public body that provides healthcare to all permanent residents in England, that is free at the point of use. The body is one of four forming the UK National Health Service as health is a devolved matter; there are differences with the provisions for healthcare elsewhere in the United Kingdom, and in England it is overseen by NHS England. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing and able to pay.

Healthcare in Scotland is mainly provided by Scotland's public health service, NHS Scotland. It provides healthcare to all permanent residents free at the point of need and paid for from general taxation. Health is a matter that is devolved, and considerable differences have developed between the public healthcare systems in the countries of the United Kingdom, collectively the National Health Service (NHS). Though the public system dominates healthcare provision, private healthcare and a wide variety of alternative and complementary treatments are available for those willing and able to pay.

Healthcare in Wales is mainly provided by the Welsh public health service, NHS Wales. NHS Wales provides healthcare to all permanent residents that is free at the point of need and paid for from general taxation. Health is a matter that is devolved, and considerable differences are now developing between the public healthcare systems in the different countries of the United Kingdom, collectively the National Health Service (NHS). Though the public system dominates healthcare provision, private health care and a wide variety of alternative and complementary treatments are available for those willing to pay.

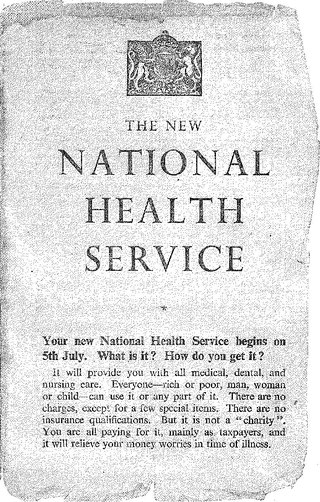
The National Health Service (NHS) is the umbrella term for the publicly funded healthcare systems of the United Kingdom, comprising the National Health Service in England, NHS Scotland and NHS Wales. Health and Social Care in Northern Ireland was created separately and is often locally referred to as "the NHS". The original three systems were established in 1948 as part of major social reforms following the Second World War. The founding principles were that services should be comprehensive, universal and free at the point of delivery—a health service based on clinical need, not ability to pay. Each service provides a comprehensive range of health services, provided without charge for people ordinarily resident in the United Kingdom apart from dental treatment and optical care. In England, NHS patients have to pay prescription charges; some, such as those aged over 60, or those on certain state benefits, are exempt.
NHS targets are performance measures used by NHS England, NHS Scotland, NHS Wales, and the Health and Social Care service in Northern Ireland. These vary by country but assess the performance of each health service against measures such as 5 hour waiting times in Accident and Emergency departments, weeks to receive an appointment and/or treatment, and performance in specific departments such as oncology.
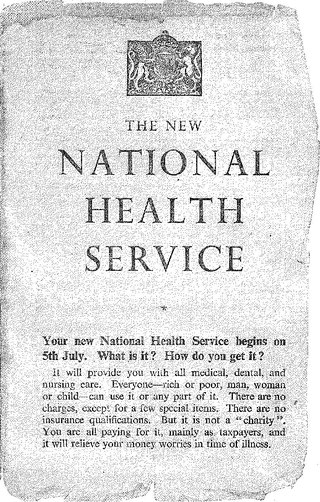
The National Health Service in England was created by the National Health Service Act 1946. Responsibility for the NHS in Wales was passed to the Secretary of State for Wales in 1969, leaving the Secretary of State for Social Services responsible for the NHS in England by itself.
NHS Scotland is the publicly funded healthcare systems in Scotland. It was founded by the National Health Service (Scotland) Act 1947 and was launched on 5 July 1948, under the control of the Secretary of State for Scotland. As a result of the Scotland Act 1998, control over NHS Scotland transferred to the Scottish Government and Parliament in 1999.
111 is a free-to-call single non-emergency number medical helpline operating in England, Scotland and Wales. The 111 phone service has replaced the various non-geographic 0845 rate numbers and is part of each country's National Health Service: in England the service is known as NHS 111; in Scotland, NHS 24; and in Wales, NHS111 Wales.
Examples of health care systems of the world, sorted by continent, are as follows.
Dentistry provided by the National Health Service in the United Kingdom is supposed to ensure that dental treatment is available to the whole population. Most dentistry is provided by private practitioners, most of whom also provide, on a commercial basis, services which the NHS does not provide, largely cosmetic. Most adult patients have to pay some NHS charges, although these are often significantly cheaper than the cost of private dentistry. The majority of people choose NHS dental care rather than private care: as of 2005, the national average proportion of people opting for private care was 23%. NHS dentistry is not always available and is not managed in the way that other NHS services are managed.

Private healthcare in the UK, where universal state-funded healthcare is provided by the National Health Service, is a niche market.

Health and social care on the Isle of Man is the responsibility of the Department of Health and Social Care. Healthcare in Isle of Man is free for residents and visitors from the UK, and there is a reciprocal health agreement with the UK. For several years, it has required a supplementary vote to balance its budget at the end of each year. The Reciprocal Health Agreement only covers three months from the point of arrival in the UK.
The private provision of NHS services has been considered a controversial topic since the early 1990s. Keep Our NHS Public, NHS Support Federation and other groups have campaigned against the threat of privatisation, largely in England.