The pudendal nerve is the main nerve of the perineum. It carries sensation from the external genitalia of both sexes and the skin around the anus and perineum, as well as the motor supply to various pelvic muscles, including the male or female external urethral sphincter and the external anal sphincter. If damaged, most commonly by childbirth, lesions may cause sensory loss or fecal incontinence. The nerve may be temporarily blocked as part of an anaesthetic procedure.

A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general anesthetic. When it is used on specific nerve pathways, paralysis also can be achieved.

Tietze syndrome is a benign inflammation of one or more of the costal cartilages. It was first described in 1921 by German surgeon Alexander Tietze and was subsequently named after him. The condition is characterized by tenderness and painful swelling of the anterior (front) chest wall at the costochondral, sternocostal, or sternoclavicular junctions. Tietze syndrome affects the true ribs and has a predilection for the 2nd and 3rd ribs, commonly affecting only a single joint.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés. In the United States, over 50% of childbirths involve the use of epidural anesthesia.

A thoracotomy is a surgical procedure to gain access into the pleural space of the chest. It is performed by surgeons to gain access to the thoracic organs, most commonly the heart, the lungs, or the esophagus, or for access to the thoracic aorta or the anterior spine. A thoracotomy is the first step in thoracic surgeries including lobectomy or pneumonectomy for lung cancer or to gain thoracic access in major trauma.

Costochondritis, also known as chest wall pain syndrome or costosternal syndrome, is a benign inflammation of the upper costochondral and sternocostal joints. 90% of patients are affected in multiple ribs on a single side, typically at the 2nd to 5th ribs. Chest pain, the primary symptom of costochondritis, is considered a symptom of a medical emergency, making costochondritis a common presentation in the emergency department. One study found costochondritis was responsible for 30% of patients with chest pain in an emergency department setting.

The stellate ganglion is a sympathetic ganglion formed by the fusion of the inferior cervical ganglion and the first thoracic ganglion, which exists in 80% of people. Sometimes, the second and the third thoracic ganglia are included in this fusion. The stellate ganglion is relatively big compared to much smaller thoracic, lumbar and sacral ganglia, and is polygonal in shape. Stellate ganglion is located at the level of C7, anterior to the transverse process of C7 and the neck of the first rib, superior to the cervical pleura and just below the subclavian artery. It is superiorly covered by the prevertebral lamina of the cervical fascia and anteriorly in relation with common carotid artery, subclavian artery and the beginning of vertebral artery which sometimes leaves a groove at the apex of this ganglion.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.

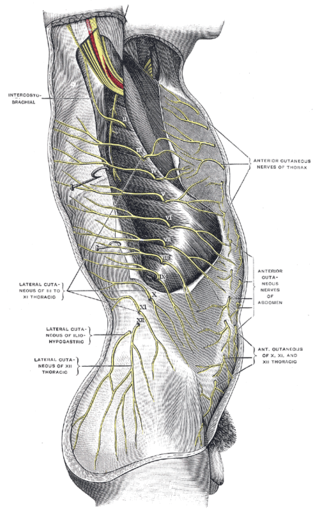
The intercostal nerves are part of the somatic nervous system, and arise from the anterior rami of the thoracic spinal nerves from T1 to T11. The intercostal nerves are distributed chiefly to the thoracic pleura and abdominal peritoneum, and differ from the anterior rami of the other spinal nerves in that each pursues an independent course without plexus formation.

A rib fracture is a break in a rib bone. This typically results in chest pain that is worse with inspiration. Bruising may occur at the site of the break. When several ribs are broken in several places a flail chest results. Potential complications include a pneumothorax, pulmonary contusion, and pneumonia.
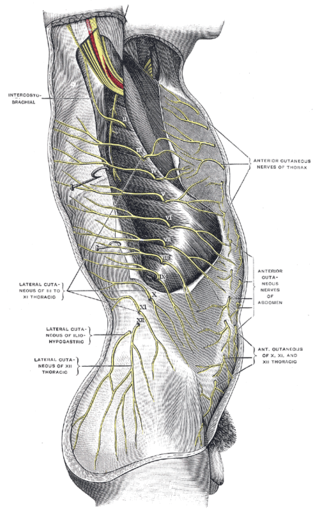
The subcostal nerve is larger than the others. It runs along the lower border of the twelfth rib, often gives a communicating branch to the first lumbar nerve, and passes under the lateral lumbocostal arch.
A retrobulbar block is a regional anesthetic nerve block in the retrobulbar space, the area located behind the globe of the eye. Injection of local anesthetic into this space constitutes the retrobulbar block. This injection provides akinesia of the extraocular muscles by blocking cranial nerves II, III, and VI, thereby preventing movement of the globe. Cranial nerve IV lies outside the muscle cone, and therefore is not affected by the local anesthesia. As a result, intorsion of the eye is still possible. It also provides sensory anesthesia of the conjunctiva, cornea and uvea by blocking the ciliary nerves. This block is most commonly employed for cataract surgery, but also provides anesthesia for other intraocular surgeries.

Brachial plexus block is a regional anesthesia technique that is sometimes employed as an alternative or as an adjunct to general anesthesia for surgery of the upper extremity. This technique involves the injection of local anesthetic agents in close proximity to the brachial plexus, temporarily blocking the sensation and ability to move the upper extremity. The subject can remain awake during the ensuing surgical procedure, or they can be sedated or even fully anesthetized if necessary.
Pain in cancer may arise from a tumor compressing or infiltrating nearby body parts; from treatments and diagnostic procedures; or from skin, nerve and other changes caused by a hormone imbalance or immune response. Most chronic (long-lasting) pain is caused by the illness and most acute (short-term) pain is caused by treatment or diagnostic procedures. However, radiotherapy, surgery and chemotherapy may produce painful conditions that persist long after treatment has ended.
Interventional pain management or interventional pain medicine is a medical subspecialty defined by the National Uniforms Claims Committee (NUCC) as, " invasive interventions such as the discipline of medicine devoted to the diagnosis and treatment of pain related disorders principally with the application of interventional techniques in managing sub acute, chronic, persistent, and intractable pain, independently or in conjunction with other modalities of treatment". Medicare Payment Advisory Commission (MedPAC) defined interventional techniques as, "minimally invasive procedures including, percutaneous precision needle placement, with placement of drugs in targeted areas or ablation of targeted nerves; and some surgical techniques such as laser or endoscopic diskectomy, intrathecal infusion pumps and spinal cord stimulators, for the diagnosis and management of chronic, persistent or intractable pain". Minimally invasive interventions such as facet joint injections, nerve blocks, neuroaugmentation, vertebroplasty, kyphoplasty, nucleoplasty, endoscopic discectomy, and implantable drug delivery systems are utilized in managing subacute or chronic pain.
Neurotomy may refer to the application of heat or freezing to sensory nerve fibers to cause their temporary degeneration, usually to relieve pain. Neurotomy and neurolysis are forms of neurolytic block. "Neurotomy" is sometimes used as a synonym for neurectomy, the surgical cutting or removal of nervous tissue.

Local anesthetic nerve block is a short-term nerve block involving the injection of local anesthetic as close to the nerve as possible for pain relief. The local anesthetic bathes the nerve and numbs the area of the body that is supplied by that nerve. The goal of the nerve block is to prevent pain by blocking the transmission of pain signals from the affected area. Nerve blocks have a number of uses including treating headache disorders and providing anesthesia during surgery. The pain relief provided by the block is present during the surgery and continues to last after the procedure. This can lead to a reduction in the amount of opiates needed for pain control. The advantages of nerve blocks over general anesthesia include faster recovery, monitored anesthesia care vs. intubation with an airway tube, and much less postoperative pain.
Phulchand Prithvi Raj was an Indian American physician and anesthesiologist specializing in interventional pain management. His name is synonymous with regional anesthesia and interventional pain management including development of multiple training programs, training of thousands of individual physicians, numerous publications, and organization of interventional pain management as a distinct specialty. Some felt his passing created a void in interventional pain management across the globe. Some of his major contributions during his career involved the development and implementation of regional anesthesia and interventional pain management.

Iliocostal friction syndrome, also known as costoiliac impingement syndrome, is a condition in which the costal margin comes in contact with the iliac crest. The condition presents as low back pain which may radiate to other surrounding areas as a result of irritated nerve, tendon, and muscle structures. It may occur unilaterally due to conditions such as scoliosis, or bilaterally due to conditions such as osteoporosis and hyperkyphosis.