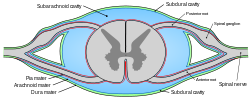
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
General anaesthetics are often defined as compounds that induce a loss of consciousness in humans or loss of righting reflex in animals. Clinical definitions are also extended to include an induced coma that causes lack of awareness to painful stimuli, sufficient to facilitate surgical applications in clinical and veterinary practice. General anaesthetics do not act as analgesics and should also not be confused with sedatives. General anaesthetics are a structurally diverse group of compounds whose mechanisms encompass multiple biological targets involved in the control of neuronal pathways. The precise workings are the subject of some debate and ongoing research.

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients. Depending on the procedure, general anaesthesia may be optional or required. Regardless of whether a patient may prefer to be unconscious or not, certain pain stimuli could result in involuntary responses from the patient that may make an operation extremely difficult. Thus, for many procedures, general anaesthesia is required from a practical perspective.

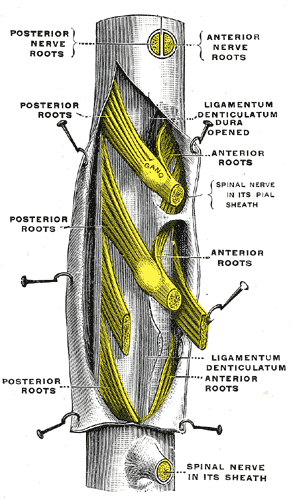
Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opiod into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Combined spinal and epidural anaesthesia is a regional anaesthetic technique, which combines the benefits of both spinal anaesthesia and epidural anaesthesia and analgesia. The spinal component gives a rapid onset of a predictable block. The indwelling epidural catheter gives the ability to provide long lasting analgesia and to titrate the dose given to the desired effect.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.
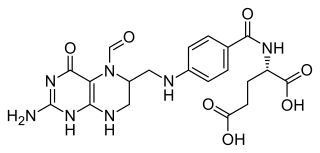
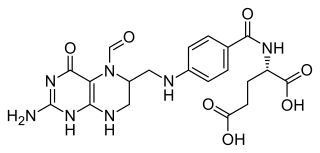
Folinic acid, also known as leucovorin, is a medication used to decrease the toxic effects of methotrexate and pyrimethamine. It is also used in combination with 5-fluorouracil to treat colorectal cancer and pancreatic cancer, may be used to treat folate deficiency that results in anemia, and methanol poisoning. It is taken by mouth, injection into a muscle, or injection into a vein.
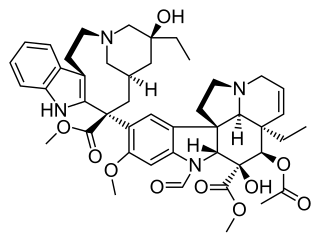
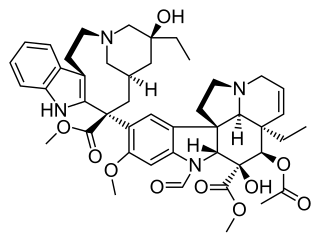
Vincristine, also known as leurocristine and marketed under the brand name Oncovin among others, is a chemotherapy medication used to treat a number of types of cancer. This includes acute lymphocytic leukemia, acute myeloid leukemia, Hodgkin's disease, neuroblastoma, and small cell lung cancer among others. It is given intravenously.

Baclofen, sold under the brand name Lioresal among others, is a medication used to treat muscle spasticity such as from a spinal cord injury or multiple sclerosis. It may also be used for hiccups and muscle spasms near the end of life, and off-label to treat alcohol use disorder or opioid withdrawal symptoms. It is taken orally or by intrathecal pump. It is also sometimes used transdermally in combination with gabapentin and clonidine prepared at a compounding pharmacy.

Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease sensation in a specific small area. In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal's epidural space. It is available mixed with a small amount of epinephrine to increase the duration of its action. It typically begins working within 15 minutes and lasts for 2 to 8 hours.
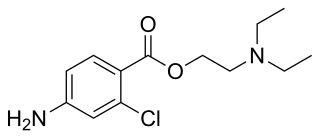
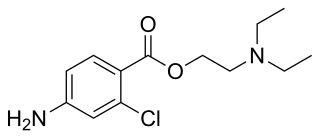
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.
An intrathecal pump is a medical device used to deliver medications directly into the space between the spinal cord and the protective sheath surrounding the spinal cord. Medications such as baclofen, bupivacaine, clonidine, morphine, hydromorphone, fentanyl or ziconotide may be delivered in this manner to minimize the side effects often associated with the higher doses used in oral or intravenous delivery of these drugs.
Toxic leukoencephalopathy is a rare condition that is characterized by progressive damage (-pathy) to white matter (-leuko-) in the brain (-encephalo-), particularly myelin, due to causes such as exposure to substance use, environmental toxins, or chemotherapeutic drugs. The prevalence of this disease is infrequent and often goes unreported, especially in cases resulting from substance use. Magnetic resonance imaging (MRI) is a popular method to study and diagnose the disease. However, even with technological advances, the exact mechanism and underlying pathophysiology of toxic leukoencephalopathy remains unknown and is thought to vary between sources of toxicity. The clinical severity of toxic leukoencephalopathy also varies among patients, exposure time, concentration, and purity of the toxic agent. Some reversibility of the condition has been seen in many cases when the toxic agent is removed.
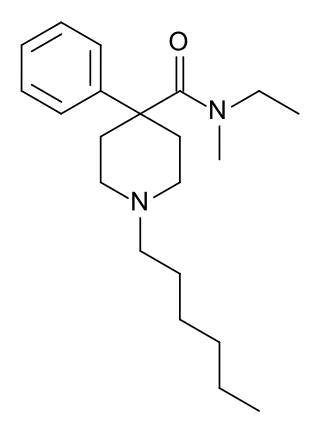
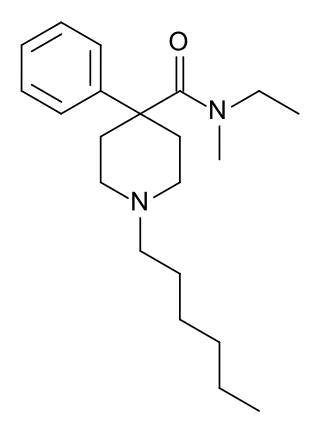
Sameridine is a 4-phenylpiperidine derivative that is related to the opioid analgesic drug pethidine (meperidine).

Leptomeningeal cancer is a rare complication of cancer in which the disease spreads from the original tumor site to the meninges surrounding the brain and spinal cord. This leads to an inflammatory response, hence the alternative names neoplastic meningitis (NM), malignant meningitis, or carcinomatous meningitis. The term leptomeningeal describes the thin meninges, the arachnoid and the pia mater, between which the cerebrospinal fluid is located. The disorder was originally reported by Eberth in 1870. It is also known as leptomeningeal carcinomatosis, leptomeningeal disease (LMD), leptomeningeal metastasis, meningeal metastasis and meningeal carcinomatosis.
Drug-Induced Aseptic Meningitis (DIAM) is a type of aseptic meningitis related to the use of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or biologic drugs such as intravenous immunoglobulin (IVIG). Additionally, this condition generally shows clinical improvement after cessation of the medication, as well as a tendency to relapse with resumption of the medication.
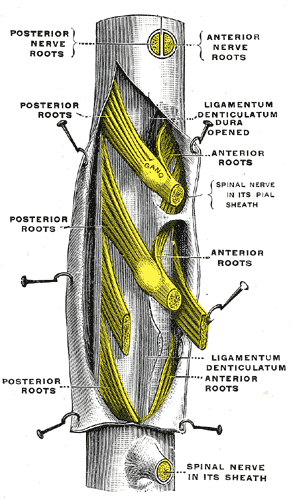
The thecal sac or dural sac is the membranous sheath (theca) or tube of dura mater that surrounds the spinal cord and the cauda equina. The thecal sac contains the cerebrospinal fluid which provides nutrients and buoyancy to the spinal cord. From the skull the tube adheres to bone at the foramen magnum and extends down to the second sacral vertebra where it tapers to cover over the filum terminale. Along most of the spinal canal it is separated from the inner surface by the epidural space. The sac has projections that follow the spinal nerves along their paths out of the vertebral canal which become the dural root sheaths.

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults, it can be used in the context of anorectal surgery or for chronic low back pain management.
Central Nervous System Prophylaxis, or CNS prophylaxis, is a type of chemotherapy for patients at risk of cancer metastasis into the central nervous system (CNS). Prophylaxis originated from the Greek word “phulaxis”, meaning the act of guarding. CNS prophylaxis refers to preventative measures that kill cancer cells potentially in the intrathecal space and the organs of the central nervous system.