Related Research Articles

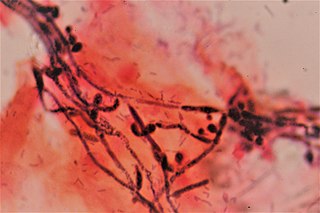
Candidiasis is a fungal infection due to any type of Candida. When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing. When it affects the vagina, it may be referred to as a yeast infection or thrush. Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Yeast infections of the penis are less common and typically present with an itchy rash. Very rarely, yeast infections may become invasive, spreading to other parts of the body. This may result in fevers along with other symptoms depending on the parts involved.
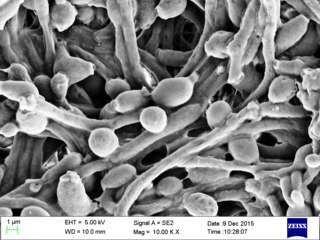
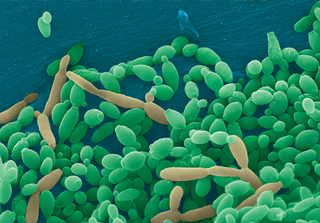
Candida albicans is an opportunistic pathogenic yeast that is a common member of the human gut flora. It can also survive outside the human body. It is detected in the gastrointestinal tract and mouth in 40–60% of healthy adults. It is usually a commensal organism, but it can become pathogenic in immunocompromised individuals under a variety of conditions. It is one of the few species of the genus Candida that cause the human infection candidiasis, which results from an overgrowth of the fungus. Candidiasis is, for example, often observed in HIV-infected patients. C. albicans is the most common fungal species isolated from biofilms either formed on (permanent) implanted medical devices or on human tissue. C. albicans, C. tropicalis, C. parapsilosis, and C. glabrata are together responsible for 50–90% of all cases of candidiasis in humans. A mortality rate of 40% has been reported for patients with systemic candidiasis due to C. albicans. By one estimate, invasive candidiasis contracted in a hospital causes 2,800 to 11,200 deaths yearly in the US. Nevertheless, these numbers may not truly reflect the true extent of damage this organism causes, given new studies indicating that C. albicans can cross the blood–brain barrier in mice.

An antifungal medication, also known as an antimycotic medication, is a pharmaceutical fungicide or fungistatic used to treat and prevent mycosis such as athlete's foot, ringworm, candidiasis (thrush), serious systemic infections such as cryptococcal meningitis, and others. Such drugs are usually obtained by a doctor's prescription, but a few are available over the counter (OTC). The evolution of antifungal resistance is a growing threat to health globally.
Candida is a genus of yeasts and is the most common cause of fungal infections worldwide. In fact, it is the largest genus of medically important yeasts.

Fluconazole is an antifungal medication used for a number of fungal infections. This includes candidiasis, blastomycosis, coccidioidomycosis, cryptococcosis, histoplasmosis, dermatophytosis, and pityriasis versicolor. It is also used to prevent candidiasis in those who are at high risk such as following organ transplantation, low birth weight babies, and those with low blood neutrophil counts. It is given either by mouth or by injection into a vein.

Oral candidiasis, also known as oral thrush among other names, is candidiasis that occurs in the mouth. That is, oral candidiasis is a mycosis of Candida species on the mucous membranes of the mouth.

Fungal infection, also known as mycosis, is a disease caused by fungi. Different types are traditionally divided according to the part of the body affected; superficial, subcutaneous, and systemic. Superficial fungal infections include common tinea of the skin, such as tinea of the body, groin, hands, feet and beard, and yeast infections such as pityriasis versicolor. Subcutaneous types include eumycetoma and chromoblastomycosis, which generally affect tissues in and beneath the skin. Systemic fungal infections are more serious and include cryptococcosis, histoplasmosis, pneumocystis pneumonia, aspergillosis and mucormycosis. Signs and symptoms range widely. There is usually a rash with superficial infection. Fungal infection within the skin or under the skin may present with a lump and skin changes. Pneumonia-like symptoms or meningitis may occur with a deeper or systemic infection.

Caspofungin is a lipopeptide antifungal drug from Merck & Co., Inc. discovered by James Balkovec, Regina Black and Frances A. Bouffard. It is a member of a new class of antifungals termed the echinocandins. It works by inhibiting the enzyme (1→3)-β-D-glucan synthase and thereby disturbing the integrity of the fungal cell wall. Caspofungin was the first inhibitor of fungal (1→3)-β-D-glucan synthesis to be approved by the United States Food and Drug Administration. Caspofungin is administered intravenously.

Fungal pneumonia is an infection of the lungs by fungi. It can be caused by either endemic or opportunistic fungi or a combination of both. Case mortality in fungal pneumonias can be as high as 90% in immunocompromised patients, though immunocompetent patients generally respond well to anti-fungal therapy.
Fungemia is the presence of fungi or yeasts in the blood. The most common type, also known as candidemia, candedemia, or systemic candidiasis, is caused by Candida species; candidemia is also among the most common bloodstream infections of any kind. Infections by other fungi, including Saccharomyces, Aspergillus and Cryptococcus, are also called fungemia. It is most commonly seen in immunosuppressed or immunocompromised patients with severe neutropenia, cancer patients, or in patients with intravenous catheters. It has been suggested that otherwise immunocompetent patients taking infliximab may also be at a higher risk for fungemia.

Anidulafungin (INN) is a semisynthetic echinocandin used as an antifungal drug. It was previously known as LY303366. It may also have application in treating invasive Aspergillus infection when used in combination with voriconazole. It is a member of the class of antifungal drugs known as the echinocandins; its mechanism of action is by inhibition of (1→3)-β-D-glucan synthase, an enzyme important to the synthesis of the fungal cell wall.
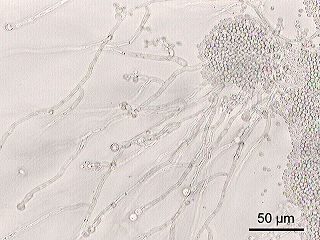
Candida parapsilosis is a fungal species of yeast that has become a significant cause of sepsis and of wound and tissue infections in immunocompromised people. Unlike Candida albicans and Candida tropicalis, C. parapsilosis is not an obligate human pathogen, having been isolated from nonhuman sources such as domestic animals, insects and soil. C. parapsilosis is also a normal human commensal and it is one of the fungi most frequently isolated from human hands. There are several risk factors that can contribute to C. parapsilosis colonization. Immunocompromised individuals and surgical patients, particularly those undergoing surgery of the gastrointestinal tract, are at high risk for infection with C. parapsilosis. There is currently no consensus on the treatment of invasive candidiasis caused by C. parapsilosis, although the therapeutic approach typically includes the removal of foreign bodies such as implanted prostheses and the administration of systemic antifungal therapy. Amphotericin B and Fluconazole are often used in the treatment of C. parapsilosis infection.
Candida krusei is a budding yeast involved in chocolate production. Candida krusei is an emerging fungal nosocomial pathogen primarily found in the immunocompromised and those with hematological malignancies. It has natural resistance to fluconazole, a standard antifungal agent. It is most often found in patients who have had prior fluconazole exposure, sparking debate and conflicting evidence as to whether fluconazole should be used prophylactically. Mortality due to C. krusei fungemia is much higher than the more common C. albicans. Other Candida species that also fit this profile are C. parapsilosis, C. glabrata, C. tropicalis, C. guillermondii and C. rugosa. Candida krusei is the anamorph name; the teleomorph name for the same organism is Pichia kudriavzevii. The International Commission on the Taxonomy of Fungi (ICTF) and the Nomenclature Committee for Fungi (NCF) have proposed revising the standard name to Pichia kudriavzevii in 2021.
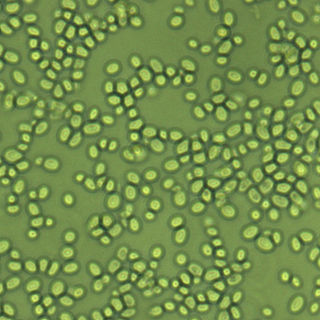
Candida glabrata is a species of haploid yeast of the genus Candida, previously known as Torulopsis glabrata. Despite the fact that no sexual life cycle has been documented for this species, C. glabrata strains of both mating types are commonly found. C. glabrata is generally a commensal of human mucosal tissues, but in today's era of wider human immunodeficiency from various causes, C. glabrata is often the second or third most common cause of candidiasis as an opportunistic pathogen. Infections caused by C. glabrata can affect the urogenital tract or even cause systemic infections by entrance of the fungal cells in the bloodstream (Candidemia), especially prevalent in immunocompromised patients.
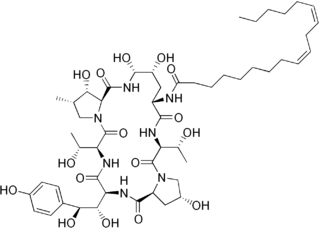
Echinocandins are a class of antifungal drugs that inhibit the synthesis of β-glucan in the fungal cell wall via noncompetitive inhibition of the enzyme 1,3-β glucan synthase. The class has been termed the "penicillin of antifungals," along with the related papulacandins, as their mechanism of action resembles that of penicillin in bacteria. β-glucans are carbohydrate polymers that are cross-linked with other fungal cell wall components, the fungal equivalent to bacterial peptidoglycan. Caspofungin, micafungin, and anidulafungin are semisynthetic echinocandin derivatives with limited clinical use due to their solubility, antifungal spectrum, and pharmacokinetic properties.
Pathogenic fungi are fungi that cause disease in humans or other organisms. Although fungi are eukaryotic, many pathogenic fungi are microorganisms. Approximately 300 fungi are known to be pathogenic to humans; their study is called "medical mycology". Fungal infections kill more people than either tuberculosis or malaria—about 2 million people per year.
Vaginal yeast infection, also known as candidal vulvovaginitis and vaginal thrush, is excessive growth of yeast in the vagina that results in irritation. The most common symptom is vaginal itching, which may be severe. Other symptoms include burning with urination, a thick, white vaginal discharge that typically does not smell bad, pain during sex, and redness around the vagina. Symptoms often worsen just before a woman's period.

Candida auris is a species of fungus that grows as yeast. It is one of the few species of the genus Candida which cause candidiasis in humans. Often, candidiasis is acquired in hospitals by patients with weakened immune systems. C. auris can cause invasive candidiasis (fungemia) in which the bloodstream, the central nervous system, and internal organs are infected. It has attracted widespread attention because of its multiple drug resistance. Treatment is also complicated because it is easily misidentified as other Candida species.
Candida tropicalis is a species of yeast in the genus Candida. It is a common pathogen in neutropenic hosts, in whom it may spread through the bloodstream to peripheral organs. For invasive disease, treatments include amphotericin B, echinocandins, or extended-spectrum triazole antifungals.
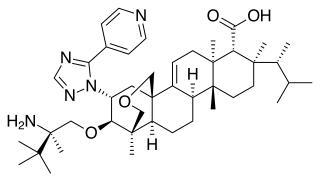
Ibrexafungerp, sold under the brand name Brexafemme, is an antifungal medication used to treat vulvovaginal candidiasis (VVC). It is taken orally. It is also currently undergoing clinical trials for other indications via an intravenous (IV) formulation. An estimated 75% of women will have at least one episode of VVC and 40 to 45% will have two or more episodes in their lifetime.
References
- ↑ "Invasive Candidiasis | Candidiasis | Types of Fungal Diseases | Fungal Diseases | CDC". www.cdc.gov. Retrieved 2017-04-02.
- 1 2 3 4 5 6 7 "Candidiasis (Invasive) – Infectious Diseases". MSD Manual Professional Edition. Retrieved 2017-04-06.
- ↑ "Symptoms | Invasive Candidiasis | Candidiasis | Types of Diseases | Fungal Diseases | CDC". www.cdc.gov. Retrieved 2017-04-03.
- 1 2 3 4 5 Yapar, Nur (2014-01-01). "Epidemiology and risk factors for invasive candidiasis". Therapeutics and Clinical Risk Management. 10: 95–105. doi: 10.2147/TCRM.S40160 . ISSN 1176-6336. PMC 3928396 . PMID 24611015.
- ↑ "Fatal Fungus Linked to 4 New Deaths – What You Need to Know". 2016-11-07. Retrieved 2017-04-04.
- 1 2 3 4 5 6 7 8 9 10 "Clinical Alert to U.S. Healthcare Facilities – Fungal Diseases | CDC". www.cdc.gov. June 2016. Retrieved 2017-04-06.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Kullberg, Bart Jan; Arendrup, Maiken C. (2015-10-08). "Invasive Candidiasis". The New England Journal of Medicine. 373 (15): 1445–1456. doi:10.1056/NEJMra1315399. hdl: 2066/152392 . ISSN 1533-4406. PMID 26444731. S2CID 43788.
- ↑ "Diagnosis and Testing | Invasive Candidiasis | Candidiasis | Types of Diseases | Fungal Diseases | CDC". www.cdc.gov. Retrieved 2017-04-03.
- ↑ Vincenzi, V.; Fioroni, E.; Benvegnù, B.; De Angelis, M.; Bartolucci, L.; Gradoli, C.; Valori, C. (1985-05-12). "[Effects of calcium antagonists on pancreatic endocrine secretion]". Minerva Medica. 76 (19–20): 919–921. ISSN 0026-4806. PMID 3889722.
- 1 2 "Treatment | Invasive Candidiasis | Candidiasis | Types of Diseases | Fungal Diseases | CDC". www.cdc.gov. Retrieved 2017-04-03.
- 1 2 3 4 "Statistics | Invasive Candidiasis | Candidiasis | Types of Diseases | Fungal Diseases | CDC". www.cdc.gov. Retrieved 2017-04-03.