Acupuncture is a form of alternative medicine and a component of traditional Chinese medicine (TCM) in which thin needles are inserted into the body. Acupuncture is a pseudoscience; the theories and practices of TCM are not based on scientific knowledge, and it has been characterized as quackery.

Interstitial cystitis (IC), a type of bladder pain syndrome (BPS), is chronic pain in the bladder and pelvic floor of unknown cause. It is the urologic chronic pelvic pain syndrome of women. Symptoms include feeling the need to urinate right away, needing to urinate often, and pain with sex. IC/BPS is associated with depression and lower quality of life. Many of those affected also have irritable bowel syndrome and fibromyalgia.
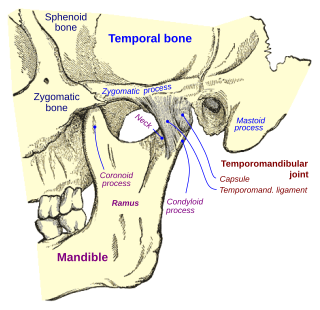
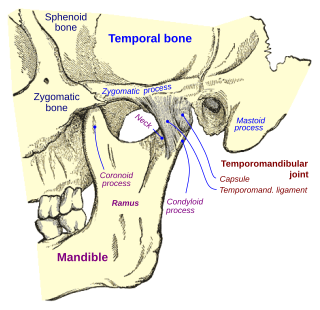
Temporomandibular joint dysfunction is an umbrella term covering pain and dysfunction of the muscles of mastication and the temporomandibular joints. The most important feature is pain, followed by restricted mandibular movement, and noises from the temporomandibular joints (TMJ) during jaw movement. Although TMD is not life-threatening, it can be detrimental to quality of life; this is because the symptoms can become chronic and difficult to manage.

Massage is the rubbing or kneading of the body's soft tissues. Massage techniques are commonly applied with hands, fingers, elbows, knees, forearms, feet or a device. The purpose of massage is generally for the treatment of body stress or pain. In European countries, a person professionally trained to give massages is traditionally known as a masseur (male) or masseuse (female). In the United States, these individuals are often referred to as "massage therapists". In some provinces of Canada, they are called "registered massage therapists."
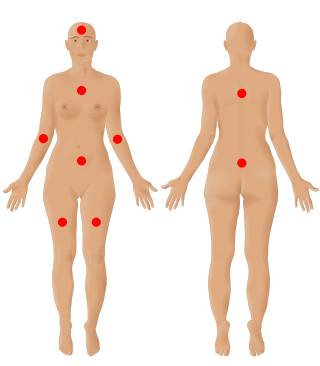
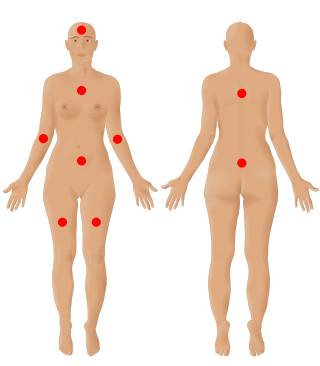
Fibromyalgia is a medical condition which causes chronic widespread pain, accompanied by fatigue, waking unrefreshed, and cognitive symptoms. Other symptoms include headaches, lower abdominal pain or cramps, and depression. People with fibromyalgia can also experience insomnia and a general hypersensitivity.

Janet Graham Travell was an American physician and medical researcher.
A microcurrent electrical neuromuscular stimulator or MENS is a device used to send weak electrical signals into the body. Such devices apply extremely small microamp [uA] electrical currents to the tissues using electrodes placed on the skin. One microampere [uA] is 1 millionth of an ampere and the uses of MENS are distinct from those of "TENS" which runs at one milliamp [mA] or one thousandth of an amp.

Plantar fasciitis or plantar heel pain is a disorder of the plantar fascia, which is the connective tissue which supports the arch of the foot. It results in pain in the heel and bottom of the foot that is usually most severe with the first steps of the day or following a period of rest. Pain is also frequently brought on by bending the foot and toes up towards the shin. The pain typically comes on gradually, and it affects both feet in about one-third of cases.

Piriformis syndrome is a condition which is believed to result from nerve compression at the sciatic nerve by the piriformis muscle. It is a specific case of deep gluteal syndrome. The largest and most bulky nerve in the human body is the sciatic nerve. Starting at its origin it is 2 cm wide and 0.5 cm thick. The sciatic nerve forms the roots of L4-S3 segments of the lumbosacral plexus. The nerve will pass inferiorly to the piriformis muscle, in the direction of the lower limb where it divides into common tibial and fibular nerves. Symptoms may include pain and numbness in the buttocks and down the leg. Often symptoms are worsened with sitting or running.
Manual therapy, or manipulative therapy, is a physical treatment primarily used by physical therapists, occupational therapists to treat musculoskeletal pain and disability; it mostly includes kneading and manipulation of muscles, joint mobilization and joint manipulation. It is also used by Rolfers, massage therapists, athletic trainers, osteopaths, and physicians.

Costochondritis, also known as chest wall pain syndrome or costosternal syndrome, is a benign inflammation of the upper costochondral and sternocostal joints. 90% of patients are affected in multiple ribs on a single side, typically at the 2nd to 5th ribs. Chest pain, the primary symptom of costochondritis, is considered a symptom of a medical emergency, making costochondritis a common presentation in the emergency department. One study found costochondritis was responsible for 30% of patients with chest pain in an emergency department setting.
Epicondylitis is the inflammation of an epicondyle or of adjacent tissues. Epicondyles are on the medial and lateral aspects of the elbow, consisting of the two bony prominences at the distal end of the humerus. These bony projections serve as the attachment point for the forearm musculature. Inflammation to the tendons and muscles at these attachment points can lead to medial and/or lateral epicondylitis. This can occur through a range of factors that overuse the muscles that attach to the epicondyles, such as sports or job-related duties that increase the workload of the forearm musculature and place stress on the elbow. Lateral epicondylitis is also known as “Tennis Elbow” due to its sports related association to tennis athletes, while medial epicondylitis is often referred to as “golfer's elbow.”

Fear of needles, known in medical literature as needle phobia, is the extreme fear of medical procedures involving injections or hypodermic needles. This can lead to avoidance of medical care and vaccine hesitancy.
Myofascial pain syndrome (MPS), also known as chronic myofascial pain (CMP), is a syndrome characterized by chronic pain in multiple myofascial trigger points ("knots") and fascial constrictions. It can appear in any body part. Symptoms of a myofascial trigger point include: focal point tenderness, reproduction of pain upon trigger point palpation, hardening of the muscle upon trigger point palpation, pseudo-weakness of the involved muscle, referred pain, and limited range of motion following approximately 5 seconds of sustained trigger point pressure.
Counterstrain is a technique used in osteopathic medicine, osteopathy, physical therapy, massage therapy, and chiropractic to treat somatic dysfunction. It is a system of diagnosis and treatment that uses tender points, which are produced by trauma, inflammation, postural strain, or disease, to identify structures to manipulate. The manipulation uses light pressure to decompress the local nociceptors and mechanoreceptors responsible for the sensation of pain, returning central sensitization to its normal state. This technique extends Strain-counterstrain, a technique inhibits the reflexes by putting the tissues in a position of ease directly opposite to that of the reflex. Strain-counterstrain is also known as the Jones technique,, and spontaneous release by position. Counterstrain was developed by Lawrence Jones in 1955 and was originally called “Spontaneous Release by Positioning,” before being termed “strain-counterstrain.”
Dry needling, also known as trigger point dry needling and intramuscular stimulation, is a treatment technique used by various healthcare practitioners, including physical therapists, physicians, and chiropractors, among others. Acupuncturists usually maintain that dry needling is adapted from acupuncture, but others consider dry needling as a variation of trigger point injections. It involves the use of either solid filiform needles or hollow-core hypodermic needles for therapy of muscle pain, including pain related to myofascial pain syndrome. Dry needling is mainly used to treat myofascial trigger points, but it is also used to target connective tissue, neural ailments, and muscular ailments. The American Physical Therapy Association defines dry needling as a technique used to treat dysfunction of skeletal muscle and connective tissue, minimize pain, and improve or regulate structural or functional damage.
Myotherapy is a form of muscle therapy which focuses on the assessment, treatment and rehabilitation of musculoskeletal pain and associated pathologies. The term myotherapy was coined by Bonnie Prudden to describe a specific type of trigger point therapy which she developed in the 1970s based on the earlier work of Travell and Simons who researched the cause and treatment of pain arising from myofascial trigger points. While based on rational principles, there is little scientific research regarding the efficacy of this therapy, so it remains controversial within the medical and academic disciplines.
Dentomandibular sensorimotor dysfunction (DMSD) is a medical condition involving the mandible, upper three cervical (neck) vertebrae, and the surrounding muscle and nerve areas.
Fu's Subcutaneous Needle (FSN), invented by Dr. Zhonghua Fu in 1996, is a method for the treatment of myofascial pain and trigger points related to Traditional Chinese Medicine (TCM) and invented by Dr. D. Simons and Dr. Janet G. Travell.

Iliocostal friction syndrome, also known as costoiliac impingement syndrome, is a condition in which the costal margin comes in contact with the iliac crest. The condition presents as low back pain which may radiate to other surrounding areas as a result of irritated nerve, tendon, and muscle structures. It may occur unilaterally due to conditions such as scoliosis, or bilaterally due to conditions such as osteoporosis and hyperkyphosis.