Bile, or gall, is a yellow-green fluid produced by the liver of most vertebrates that aids the digestion of lipids in the small intestine. In humans, bile is primarily composed of water, produced continuously by the liver, and stored and concentrated in the gallbladder. After a human eats, this stored bile is discharged into the first section of their small intestine.

A gallstone is a stone formed within the gallbladder from precipitated bile components. The term cholelithiasis may refer to the presence of gallstones or to any disease caused by gallstones, and choledocholithiasis refers to the presence of migrated gallstones within bile ducts.

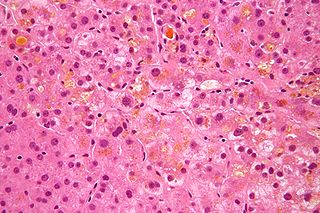
Primary biliary cholangitis (PBC), previously known as primary biliary cirrhosis, is an autoimmune disease of the liver. It results from a slow, progressive destruction of the small bile ducts of the liver, causing bile and other toxins to build up in the liver, a condition called cholestasis. Further slow damage to the liver tissue can lead to scarring, fibrosis, and eventually cirrhosis.

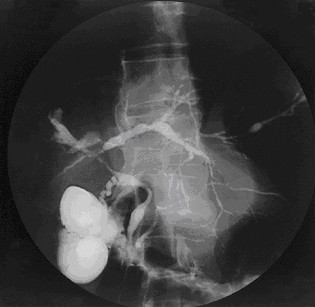
Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and pancreas so they can be seen on radiographs.
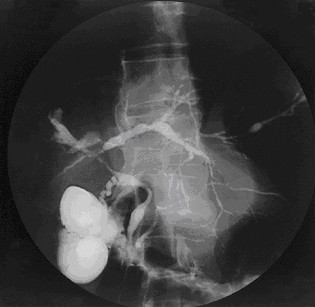
Primary sclerosing cholangitis (PSC) is a long-term progressive disease of the liver and gallbladder characterized by inflammation and scarring of the bile ducts, which normally allow bile to drain from the gallbladder. Affected individuals may have no symptoms or may experience signs and symptoms of liver disease, such as yellow discoloration of the skin and eyes, itching, and abdominal pain.

Liver disease, or hepatic disease, is any of many diseases of the liver. If long-lasting it is termed chronic liver disease. Although the diseases differ in detail, liver diseases often have features in common.

Cholangiocarcinoma, also known as bile duct cancer, is a type of cancer that forms in the bile ducts. Symptoms of cholangiocarcinoma may include abdominal pain, yellowish skin, weight loss, generalized itching, and fever. Light colored stool or dark urine may also occur. Other biliary tract cancers include gallbladder cancer and cancer of the ampulla of Vater.
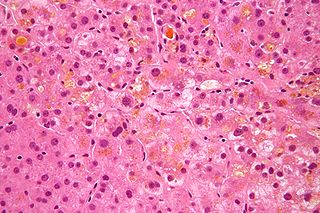
Cholestasis is a condition where the flow of bile from the liver to the duodenum is impaired. The two basic distinctions are:

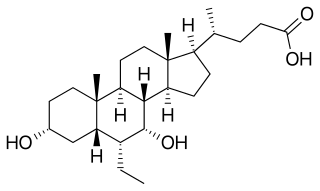
Chenodeoxycholic acid is a bile acid. Salts of this carboxylic acid are called chenodeoxycholates. Chenodeoxycholic acid is one of the main bile acids. It was first isolated from the bile of the domestic goose, which gives it the "cheno" portion of its name.

Bile acids are steroid acids found predominantly in the bile of mammals and other vertebrates. Diverse bile acids are synthesized in the liver. Bile acids are conjugated with taurine or glycine residues to give anions called bile salts.
Progressive familial intrahepatic cholestasis (PFIC) is a group of familial cholestatic conditions caused by defects in biliary epithelial transporters. The clinical presentation usually occurs first in childhood with progressive cholestasis. This usually leads to failure to thrive, cirrhosis, and the need for liver transplantation.

The biliary tract refers to the liver, gallbladder and bile ducts, and how they work together to make, store and secrete bile. Bile consists of water, electrolytes, bile acids, cholesterol, phospholipids and conjugated bilirubin. Some components are synthesized by hepatocytes ; the rest are extracted from the blood by the liver.

Gallbladder diseases are diseases involving the gallbladder and is closely linked to biliary disease, with the most common cause being gallstones (cholelithiasis).

Hyodeoxycholic acid, also known as 3α,6α-Dihydroxy-5β-cholan-24-oic acid or HDCA, is a secondary bile acid, one of the metabolic byproducts of intestinal bacteria. It differs from deoxycholic acid in that the 6α-hydroxyl is in the 12 position in the former. The 6α-hydroxyl group makes HDCA a hydrophilic acid, a property it shares with hyocholic acid. HDCA is present in mammalian species in different proportions. It is the main acid constituent of hog bile, and for this reason it was used industrially as precursor for steroid synthesis before total synthesis became practical.
Secondary sclerosing cholangitis (SSC) is a chronic cholestatic liver disease. SSC is a sclerosing cholangitis with a known cause. Alternatively, if no cause can be identified, then primary sclerosing cholangitis is diagnosed. SSC is an aggressive and rare disease with complex and multiple causes. It is characterized by inflammation, fibrosis, destruction of the biliary tree and biliary cirrhosis. It can be treated with minor interventions such as continued antibiotic use and monitoring, or in more serious cases, laparoscopic surgery intervention, and possibly a liver transplant.
Vanishing bile duct syndrome is a loose collection of diseases which leads to the injury to hepatic bile ducts and eventual ductopenia.

Ursodoxicoltaurine is the international nonproprietary name (INN) for the pharmaceutical form of tauroursodeoxycholic acid (TUDCA). It is also known as taurursodiol. Tauroursodeoxycholic acid is a naturally occurring hydrophilic bile acid which is the taurine conjugated form of ursodeoxycholic acid (UDCA). Humans have only trace amounts of tauroursodeoxycholic acid but bears have large amounts of tauroursodeoxycholic acid and ursodeoxycholic acid in their bile.
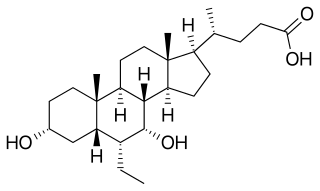
Obeticholic acid (OCA), sold under the brand name Ocaliva, is a semi-synthetic bile acid analogue which has the chemical structure 6α-ethyl-chenodeoxycholic acid. It is used as a medication used to treat primary biliary cholangitis. Intercept Pharmaceuticals Inc. hold the worldwide rights to develop OCA outside Japan and China, where it is licensed to Dainippon Sumitomo Pharma.
Intercept Pharmaceuticals, Inc. is an American biopharmaceutical company incorporated in 2002, focusing on the development of novel synthetic bile acid analogs to treat chronic liver diseases, such as primary biliary cirrhosis (PBC) now called primary biliary cholangitis, non-alcoholic fatty liver disease, cirrhosis, portal hypertension, primary sclerosing cholangitis and also the intestinal disorder, bile acid diarrhea.