Encephalitis is inflammation of the brain. The severity can be variable with symptoms including reduction or alteration in consciousness, headache, fever, confusion, a stiff neck, and vomiting. Complications may include seizures, hallucinations, trouble speaking, memory problems, and problems with hearing.
Serine is an α-amino acid that is used in the biosynthesis of proteins. It contains an α-amino group, a carboxyl group, and a side chain consisting of a hydroxymethyl group, classifying it as a polar amino acid. It can be synthesized in the human body under normal physiological circumstances, making it a nonessential amino acid. It is encoded by the codons UCU, UCC, UCA, UCG, AGU and AGC.

The N-methyl-D-aspartatereceptor (also known as the NMDA receptor or NMDAR), is a glutamate receptor and ion channel found in neurons. The NMDA receptor is one of three types of ionotropic glutamate receptors, the other two being AMPA and kainate receptors. Depending on its subunit composition, its ligands are glutamate and glycine (or D-serine). However, the binding of the ligands is typically not sufficient to open the channel as it may be blocked by Mg2+ ions which are only removed when the neuron is sufficiently depolarized. Thus, the channel acts as a “coincidence detector” and only once both of these conditions are met, the channel opens and it allows positively charged ions (cations) to flow through the cell membrane. The NMDA receptor is thought to be very important for controlling synaptic plasticity and mediating learning and memory functions.
Neuromyelitis optica spectrum disorders (NMOSD), including neuromyelitis optica (NMO), are autoimmune diseases characterized by acute inflammation of the optic nerve and the spinal cord (myelitis). Episodes of ON and myelitis can be simultaneous or successive. A relapsing disease course is common, especially in untreated patients. In more than 80% of cases, NMO is caused by immunoglobulin G autoantibodies to aquaporin 4 (anti-AQP4), the most abundant water channel protein in the central nervous system. A subset of anti-AQP4-negative cases is associated with antibodies against myelin oligodendrocyte glycoprotein (anti-MOG). Rarely, NMO may occur in the context of other autoimmune diseases or infectious diseases. In some cases, the etiology remains unknown.
Rasmussen's encephalitis is a rare inflammatory neurological disease, characterized by frequent and severe seizures, loss of motor skills and speech, hemiparesis, encephalitis, and dementia. The illness affects a single cerebral hemisphere and generally occurs in children under the age of 15.

Glutamate receptors are synaptic and non synaptic receptors located primarily on the membranes of neuronal and glial cells. Glutamate is abundant in the human body, but particularly in the nervous system and especially prominent in the human brain where it is the body's most prominent neurotransmitter, the brain's main excitatory neurotransmitter, and also the precursor for GABA, the brain's main inhibitory neurotransmitter. Glutamate receptors are responsible for the glutamate-mediated postsynaptic excitation of neural cells, and are important for neural communication, memory formation, learning, and regulation.
Experimental autoimmune encephalomyelitis, sometimes experimental allergic encephalomyelitis (EAE), is an animal model of brain inflammation. It is an inflammatory demyelinating disease of the central nervous system (CNS). It is mostly used with rodents and is widely studied as an animal model of the human CNS demyelinating diseases, including multiple sclerosis (MS) and acute disseminated encephalomyelitis (ADEM). EAE is also the prototype for T-cell-mediated autoimmune disease in general.

Meningoencephalitis, also known as herpes meningoencephalitis, is a medical condition that simultaneously resembles both meningitis, which is an infection or inflammation of the meninges, and encephalitis, which is an infection or inflammation of the brain tissue.
Inflammatory demyelinating diseases (IDDs), sometimes called Idiopathic (IIDDs) due to the unknown etiology of some of them, are a heterogenous group of demyelinating diseases - conditions that cause damage to myelin, the protective sheath of nerve fibers - that occur against the background of an acute or chronic inflammatory process. IDDs share characteristics with and are often grouped together under Multiple Sclerosis. They are sometimes considered different diseases from Multiple Sclerosis, but considered by others to form a spectrum differing only in terms of chronicity, severity, and clinical course.
Hashimoto's encephalopathy, also known as steroid-responsive encephalopathy associated with autoimmune thyroiditis (SREAT), is a neurological condition characterized by encephalopathy, thyroid autoimmunity, and good clinical response to corticosteroids. It is associated with Hashimoto's thyroiditis, and was first described in 1966. It is sometimes referred to as a neuroendocrine disorder, although the condition's relationship to the endocrine system is widely disputed. It is recognized as a rare disease by the NIH Genetic and Rare Diseases Information Center.

Limbic encephalitis is a form of encephalitis, a disease characterized by inflammation of the brain. Limbic encephalitis is caused by autoimmunity: an abnormal state where the body produces antibodies against itself. Some cases are associated with cancer and some are not. Although the disease is known as "limbic" encephalitis, it is seldom limited to the limbic system and post-mortem studies usually show involvement of other parts of the brain. The disease was first described by Brierley and others in 1960 as a series of three cases. The link to cancer was first noted in 1968 and confirmed by later investigators.
A paraneoplastic syndrome is a syndrome that is the consequence of a tumor in the body. It is specifically due to the production of chemical signaling molecules by tumor cells or by an immune response against the tumor. Unlike a mass effect, it is not due to the local presence of cancer cells.
Anti-glutamate receptor antibodies are autoantibodies detected in serum and/or cerebrospinal fluid samples of a variety of disorders such as encephalitis, epilepsy and ataxia. Clinical and experimental studies starting around the year 2000 suggest that these antibodies are not simply epiphenomena and are involved in autoimmune disease pathogenesis.

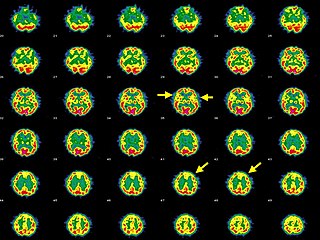
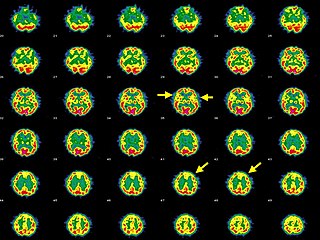
Herpes simplex encephalitis (HSE), or simply herpes encephalitis, is encephalitis due to herpes simplex virus. It is estimated to affect at least 1 in 500,000 individuals per year, and some studies suggest an incidence rate of 5.9 cases per 100,000 live births.
Bickerstaff brainstem encephalitis is a rare inflammatory disorder of the central nervous system, first described by Edwin Bickerstaff in 1951. It may also affect the peripheral nervous system, and has features in common with both Miller Fisher syndrome and Guillain–Barré syndrome.

Lymphocytic pleocytosis is an abnormal increase in the amount of lymphocytes in the cerebrospinal fluid (CSF). It is usually considered to be a sign of infection or inflammation within the nervous system, and is encountered in a number of neurological diseases, such as pseudomigraine, Susac's syndrome, and encephalitis. While lymphocytes make up roughly a quarter of all white blood cells (WBC) in the body, they are generally rare in the CSF. Under normal conditions, there are usually less than 5 white blood cells per µL of CSF. In a pleocytic setting, the number of lymphocytes can jump to more than 1,000 cells per µL. Increases in lymphocyte count are often accompanied by an increase in cerebrospinal protein concentrations in addition to pleocytosis of other types of white blood cells.

Autoimmune encephalitis (AIE) is a type of encephalitis, and one of the most common causes of noninfectious encephalitis. It can be triggered by tumors, infections, or it may be cryptogenic. The neurological manifestations can be either acute or subacute and usually develop within six weeks. The clinical manifestations include behavioral and psychiatric symptoms, autonomic disturbances, movement disorders, and seizures.
Anti-VGKC-complex encephalitis are caused by antibodies against the voltage gated potassium channel-complex (VGKC-complex) and are implicated in several autoimmune conditions including limbic encephalitis, epilepsy and neuromyotonia.
Anti-Hu associated encephalitis, also known as Anti-ANNA1 associated encephalitis, is an uncommon form of brain inflammation that is associated with an underlying cancer. It can cause psychiatric symptoms such as depression, anxiety, and hallucinations. It can also produce neurological symptoms such as confusion, memory loss, weakness, sensory loss, pain, seizures, and problems coordinating the movement of the body.
Anti-IgLON5 disease is a neurodegenerative autoimmune disease. It is marked by parasomnias and chorea - an involuntary movement disorder.