Zygomycosis is the broadest term to refer to infections caused by bread mold fungi of the zygomycota phylum. However, because zygomycota has been identified as polyphyletic, and is not included in modern fungal classification systems, the diseases that zygomycosis can refer to are better called by their specific names: mucormycosis, phycomycosis and basidiobolomycosis. These rare yet serious and potentially life-threatening fungal infections usually affect the face or oropharyngeal cavity. Zygomycosis type infections are most often caused by common fungi found in soil and decaying vegetation. While most individuals are exposed to the fungi on a regular basis, those with immune disorders (immunocompromised) are more prone to fungal infection. These types of infections are also common after natural disasters, such as tornadoes or earthquakes, where people have open wounds that have become filled with soil or vegetative matter.

Mucor is a microbial genus of approximately 40 species of molds in the family Mucoraceae. Species are commonly found in soil, digestive systems, plant surfaces, some cheeses like Tomme de Savoie, rotten vegetable matter and iron oxide residue in the biosorption process.

Basidiobolus ranarum is a filamentous fungus with worldwide distribution. The fungus was first isolated by Eidam in 1886. It can saprophytically live in the intestines of mainly cold-blooded vertebrates and on decaying fruits and soil. The fungus prefers glucose as a carbon source and grows rapidly at room temperature. Basidiobolus ranarum is also known as a cause of subcutaneous zygomycosis, usually causing granulomatous infections on a host's limbs. Infections are generally geographically limited to tropical and subtropical regions such as East and West Africa. Subcutaneous zygomycosis caused by B. ranarum is a rare disease and predominantly affects children and males. Common subcutaneous zygomycosis shows characteristic features and is relatively easy to be diagnosed; while, certain rare cases might show non-specific clinical features that might pose a difficulty on its identification. Although disease caused by this fungus is known to resolve spontaneously on its own, there are a number of treatments available.

Aeromonas hydrophila is a heterotrophic, Gram-negative, rod-shaped bacterium mainly found in areas with a warm climate. This bacterium can be found in fresh or brackish water. It can survive in aerobic and anaerobic environments, and can digest materials such as gelatin and hemoglobin. A. hydrophila was isolated from humans and animals in the 1950s. It is the best known of the species of Aeromonas. It is resistant to most common antibiotics and cold temperatures and is oxidase- and indole-positive. Aeromonas hydrophila also has a symbiotic relationship as gut flora inside of certain leeches, such as Hirudo medicinalis.

Mucor racemosus is a rapidly growing, weedy mould belonging to the division Mucoromycota. It is one of the earliest fungi to be grown in pure culture and was first isolated in 1886. It has a worldwide distribution and colonizes many habitats such as vegetational products, soil and houses. The fungus is mostly known for its ability to exhibit both filamentous and yeast-like morphologies, often referred to as dimorphism. Stark differences are seen in both forms and conditions of the environment heavily affect the phases of the M. racemosus. Like many fungi, it also reproduces both sexually and asexually. The dimorphic capacity of this species has been proposed as an important factor in its pathogenicity and has enhanced the industrial importance. This species is considered an opportunistic pathogen, generally limited to immunocompromised individuals. It also been associated with allergy and inflammations of facial sinuses. Its association with allergy has made it a common fungus used in allergen medical testing. Industrial use of the fungus is in the production of enzymes and the manufacture of certain dairy foods.

Setosphaeria rostrata is a heat tolerant fungus with an asexual reproductive form (anamorph) known as Exserohilum rostratum. This fungus is a common plant pathogen, causing leaf spots as well as crown rot and root rot in grasses. It is also found in soils and on textiles in subtropical and tropical regions. Exserohilum rostratum is one of the 35 Exserohilum species implicated uncommonly as opportunistic pathogens of humans where it is an etiologic agent of sinusitis, keratitis, skin lesions and an often fatal meningoencephalitis. Infections caused by this species are most often seen in regions with hot climates like Israel, India and the southern USA.
Lacazia is a genus of fungi containing the single species Lacazia loboi, which is responsible for Lobo's disease. It is a member of the order Onygenales.

Mucormycosis, also known as black fungus, is a serious fungal infection that comes under fulminant fungal sinusitis, usually in people who are immunocompromised. It is curable only when diagnosed early. Symptoms depend on where in the body the infection occurs. It most commonly infects the nose, sinuses, eyes and brain resulting in a runny nose, one-sided facial swelling and pain, headache, fever, blurred vision, bulging or displacement of the eye (proptosis), and tissue death. Other forms of disease may infect the lungs, stomach and intestines, and skin. The fatality rate is about 54%.

Pseudallescheria boydii is a species of fungus classified in the Ascomycota. It is associated with some forms of eumycetoma/maduromycosis and is the causative agent of pseudallescheriasis. Typically found in stagnant and polluted water, it has been implicated in the infection of immunocompromised and near-drowned pneumonia patients. Treatment of infections with P. boydii is complicated by resistance to many of the standard antifungal agents normally used to treat infections by filamentous fungi.
Saksenaea vasiformis is an infectious fungus associated with cutaneous or subcutaneous lesions following trauma. It causes opportunistic infections as the entry of the fungus is through open spaces of cutaneous barrier ranging in severity from mild to severe or fatal. It lives in soils worldwide, but is considered as a rare human pathogen since only 38 cases were reported as of 2012. Saksenaea vasiformis usually fails to sporulate on the routine culture media, creating a challenge for early diagnosis, which is essential for a good prognosis. Infections are usually treated using a combination of amphotericin B and surgery. Saksenaea vasiformis is one of the few fungi known to cause necrotizing fasciitis or "flesh-eating disease".
Rhizomucor pusillus is a species of Rhizomucor. It can cause disease in humans. R. pusillus is a grey mycelium fungi most commonly found in compost piles. Yellow-brown spores grow on a stalk to reproduce more fungal cells.

Streptococcus canis is a group G beta-hemolytic species of Streptococcus. It was first isolated in dogs, giving the bacterium its name. These bacteria are characteristically different from Streptococcus dysgalactiae, which is a human-specific group G species that has a different phenotypic chemical composition. S. canis is important to the skin and mucosal health of cats and dogs, but under certain circumstances, these bacteria can cause opportunistic infections. These infections were known to afflict dogs and cats prior to the formal description of the species in Devriese et al., 1986. However, additional studies revealed cases of infection in other mammal species, including cattle and even humans. Instances of mortality from S. canis in humans are very low with only a few reported cases, while actual instances of infection may be underreported due to mischaracterizations of the bacteria as S. dysgalactiae. This species, in general, is highly susceptible to antibiotics, and plans to develop a vaccine to prevent human infections are currently being considered.

Apophysomyces variabilis is an emerging fungal pathogen that can cause serious and sometimes fatal infection in humans. This fungus is a soil-dwelling saprobe with tropical to subtropical distribution. It is a zygomycete that causes mucormycosis, an infection in humans brought about by fungi in the order Mucorales. Infectious cases have been reported globally in locations including the Americas, Southeast Asia, India, and Australia. Apophysomyces variabilis infections are not transmissible from person to person.
Phaeohyphomycosis is a diverse group of fungal infections, caused by dematiaceous fungi whose morphologic characteristics in tissue include hyphae, yeast-like cells, or a combination of these. It can be associated with an array of melanistic filamentous fungi including Alternaria species, Exophiala jeanselmei, and Rhinocladiella mackenziei.

Lichtheimia corymbifera is a thermophilic fungus in the phylum Zygomycota. It normally lives as a saprotrophic mold, but can also be an opportunistic pathogen known to cause pulmonary, CNS, rhinocerebral, or cutaneous infections in animals and humans with impaired immunity.

Exophiala phaeomuriformis is thermophilic fungus belonging to the genus Exophiala and the family Herpotrichiellaceae. it is a member of the group of fungi known as black yeasts, and is typically found in hot and humid locations, such as saunas, bathrooms, and dishwashers. This species can cause skin infections and is typically classified as a Biosafety Risk Group 2 agent.
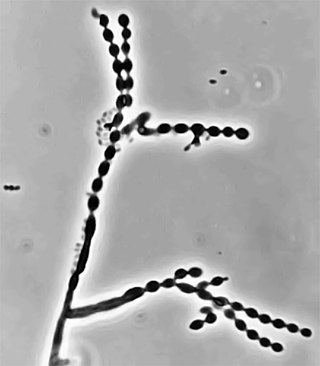
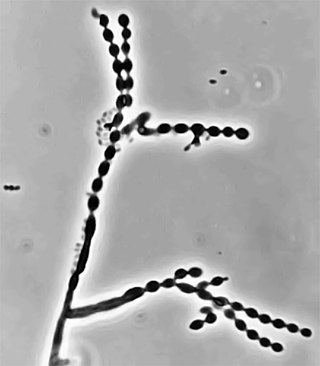
Cladophialophora is a genus of fungi in the family Herpotrichiellaceae. It has 35 species. The genus contains black yeast-like fungi, some of which are species of important medical significance. Cladophialophora bantiana causes the rare brain disease cerebral phaeohyphomycosis. Cladophialophora carrionii is a common cause of chromoblastomycosis in semi-arid climates. Some of the species are endophytes–associating with plants. For example, Cladophialophora yegresii is a cactus endophyte, which is sometimes introduced into humans via cactus spines.
Lichtheimia ramosa is a saprotrophic zygomycete, typically found in soil or dead plant material. It is a thermotolerant fungus that has also been known to act as an opportunistic pathogen–infecting both humans and animals.

Actinomucor elegans was originally described by Schostakowitsch in Siberia in 1898 and reevaluated by Benjamin and Hesseltine in 1957. Commonly found in soil and used for the commercial production of tofu and other products made by soy fermentation. Its major identifying features are its spine-like projections on the sporangiophore and its ribbon-like hyphal structure when found in the tissue of a host.

Libero Ajello was an American mycologist. He cofounded and was first president of the International Society of Human and Animal Mycology (ISHAM). He was the head of the Division of Mycotic Diseases at the Communicable Disease Center (CDC), and editor of the ISHAM Journal Medical Mycology for several years. He was one of the first researchers to investigate histoplasmosis and coccidioidomycosis in the United States and made valuable contributions to the comprehensive field of veterinary and human fungal disease diagnosis.