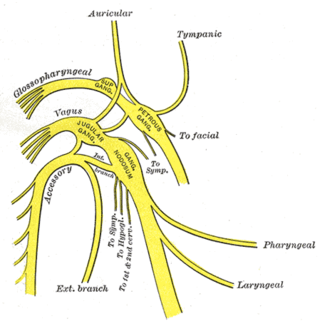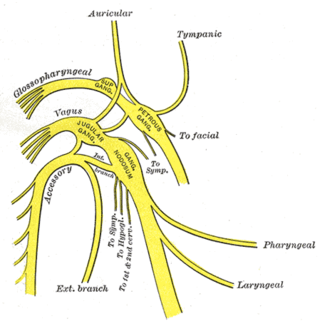
The vagus nerve, also known as the tenth cranial nerve, cranial nerve X, or simply CN X, is a cranial nerve that carries sensory fibers that create a pathway that interfaces with the parasympathetic control of the heart, lungs, and digestive tract. It comprises two nerves—the left and right vagus nerves—but they are typically referred to collectively as a single subsystem.

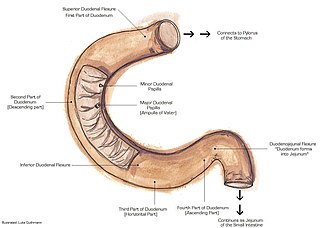
The duodenum is the first section of the small intestine in most higher vertebrates, including mammals, reptiles, and birds. In mammals it may be the principal site for iron absorption. The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine.
Articles related to anatomy include:

The phrenic nerve is a mixed motor/sensory nerve that originates from the C3-C5 spinal nerves in the neck. The nerve is important for breathing because it provides exclusive motor control of the diaphragm, the primary muscle of respiration. In humans, the right and left phrenic nerves are primarily supplied by the C4 spinal nerve, but there is also a contribution from the C3 and C5 spinal nerves. From its origin in the neck, the nerve travels downward into the chest to pass between the heart and lungs towards the diaphragm.

In human anatomy, the abdominal aorta is the largest artery in the abdominal cavity. As part of the aorta, it is a direct continuation of the descending aorta.
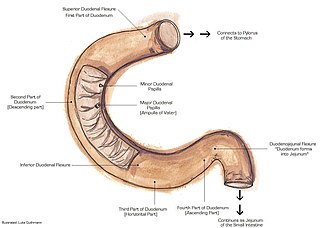
The suspensory muscle of duodenum is a thin muscle connecting the junction between the duodenum and jejunum, as well as the duodenojejunal flexure to connective tissue surrounding the superior mesenteric and coeliac arteries. The suspensory muscle most often connects to both the third and fourth parts of the duodenum, as well as the duodenojejunal flexure, although the attachment is quite variable.

The celiacartery, also known as the celiac trunk or truncus coeliacus, is the first major branch of the abdominal aorta. It is about 1.25 cm in length. Branching from the aorta at thoracic vertebra 12 (T12) in humans, it is one of three anterior/ midline branches of the abdominal aorta.
In human anatomy, the superior mesenteric artery (SMA) is an artery which arises from the anterior surface of the abdominal aorta, just inferior to the origin of the celiac trunk, and supplies blood to the intestine from the lower part of the duodenum through two-thirds of the transverse colon, as well as the pancreas.

In human anatomy, the inferior mesenteric artery (IMA) is the third main branch of the abdominal aorta and arises at the level of L3, supplying the large intestine from the distal transverse colon to the upper part of the anal canal. The regions supplied by the IMA are the descending colon, the sigmoid colon, and part of the rectum.

A nerve plexus is a plexus of intersecting nerves. A nerve plexus is composed of afferent and efferent fibers that arise from the merging of the anterior rami of spinal nerves and blood vessels. There are five spinal nerve plexuses, except in the thoracic region, as well as other forms of autonomic plexuses, many of which are a part of the enteric nervous system. The nerves that arise from the plexuses have both sensory and motor functions. These functions include muscle contraction, the maintenance of body coordination and control, and the reaction to sensations such as heat, cold, pain, and pressure. There are several plexuses in the body, including:
Neurolysis is the application of physical or chemical agents to a nerve in order to cause a temporary degeneration of targeted nerve fibers. When the nerve fibers degenerate, it causes an interruption in the transmission of nerve signals. In the medical field, this is most commonly and advantageously used to alleviate pain in cancer patients.

The abdominal aortic plexus is formed by branches derived, on either side, from the celiac plexus and ganglia, and receives filaments from some of the lumbar ganglia.

The superior hypogastric plexus is a plexus of nerves situated on the vertebral bodies anterior to the bifurcation of the abdominal aorta. It bifurcates to form the left and the right hypogastric nerve. The SHP is the continuation of the abdominal aortic plexus.

The celiac ganglia or coeliac ganglia are two large irregularly shaped masses of nerve tissue in the upper abdomen. Part of the sympathetic subdivision of the autonomic nervous system (ANS), the two celiac ganglia are the largest ganglia in the ANS, and they innervate most of the digestive tract.

The sympathetic ganglia, or paravertebral ganglia, are autonomic ganglia of the sympathetic nervous system. Ganglia are 20,000 to 30,000 afferent and efferent nerve cell bodies that run along on either side of the spinal cord. Afferent nerve cell bodies bring information from the body to the brain and spinal cord, while efferent nerve cell bodies bring information from the brain and spinal cord to the rest of the body. The cell bodies create long sympathetic chains that are on either side of the spinal cord. They also form para- or pre-vertebral ganglia of gross anatomy.

The lateral grey column is one of the three grey columns of the spinal cord ; the others being the anterior and posterior grey columns. The lateral grey column is primarily involved with activity in the sympathetic division of the autonomic motor system. It projects to the side as a triangular field in the thoracic and upper lumbar regions of the postero-lateral part of the anterior grey column.

The superior mesenteric plexus is a continuation of the lower part of the celiac plexus, receiving a branch from the junction of the right vagus nerve with the plexus.

The hepatic plexus is a sympathetic and parasympathetic nerve plexus that provides innervation to the parenchyma of the liver as well as contributing innervation to some other abdominal structures.

The following outline is provided as an overview of and topical guide to human anatomy: