| Desquamation | |
|---|---|
| Other names | Skin peeling |
 | |
| Specialty | Dermatology |
Desquamation, or peeling skin, is the shedding of dead cells from the outermost layer of skin. [1]
Contents
The term is from Latin desquamare 'to scrape the scales off a fish '.
| Desquamation | |
|---|---|
| Other names | Skin peeling |
 | |
| Specialty | Dermatology |
Desquamation, or peeling skin, is the shedding of dead cells from the outermost layer of skin. [1]
The term is from Latin desquamare 'to scrape the scales off a fish '.
Keratinocytes are the predominant cells of the epidermis, the outermost layer of the skin. Living keratinocytes reside in the basal, spinous, or granular layers of the epidermis. The outermost layer of the epidermis is called the stratum corneum and it is composed of terminally differentiated keratinocytes, the corneocytes. In the absence of disease, desquamation occurs when corneocytes are individually shed unnoticeably from the surface of the skin. [2] Typically the time it takes for a corneocyte to be formed and then shed is about 14 weeks but this time can vary depending on the anatomical location that the skin is covering. For example, desquamation occurs more slowly at acral (palm and sole) surfaces and more rapidly where the skin is thin, such as the eyelids. Normal desquamation can be visualized by immersing skin in warm or hot water. This induces the outermost layer of corneocytes to shed, such as is the case after a hot shower or bath.[ citation needed ]
Corneocytes are held together by corneodesmosomes. In order for desquamation to occur these corneodesmosome connections must be degraded. [2] Keratinocytes residing in the stratum granulosum produce corneodesmosome-degrading kallikrein family members, especially KLK1, KLK5, and KLK7. [3] Kallikreins are serine proteases. They are packaged within lamellar bodies and released into the intercellular space between the keratinocytes as they transition into becoming corneocytes. [2] To prevent premature desquamation, granular layer keratinocytes also produce kallikrein-inhibitory proteins. [3] At acral surfaces, desquamation occurs more slowly because granular layer keratinocytes downregulate expression of KLK1 and KLK7 and upregulate expression of protease inhibitors, including the KLK5-specific SPINK9 and the cysteine protease inhibitors CSTA and CST3. [3] Slowing the process of corneocyte desquamation allows acral (palm and sole) skin to form a thick protective stratum corneum. [3]
Scale forms on the skin surface in various disease settings, and is the result of abnormal desquamation. In pathologic desquamation, such as that seen in X-linked ichthyosis, the stratum corneum becomes thicker (hyperkeratosis), imparting a "dry" or scaly appearance to the skin, and instead of detaching as single cells, corneocytes are shed in clusters, which forms visible scales. [2] Desquamation of the epidermis may result from disease or injury of the skin. For example, once the rash of measles fades, there is desquamation. Skin peeling typically follows healing of a first degree burn or sunburn. Toxic shock syndrome, a potentially fatal immune system reaction to a bacterial infection such as Staphylococcus aureus , [4] can cause severe desquamation; so can mercury poisoning. Other serious skin diseases involving extreme desquamation include Stevens–Johnson syndrome and toxic epidermal necrolysis (TEN). [5] Radiation can cause dry or moist desquamation. [6] Desquamation is also abnormal in patients with immune-mediated skin diseases such as psoriasis and atopic dermatitis. [3] Abnormal desquamation often results in scale formation on the skin's surface. [3] Lipid composition alterations in scale have been used to construct diagnostic models for human skin disease. [3]
Certain eye tissues, including the conjunctiva and cornea, may undergo pathological desquamation in diseases such as dry eye syndrome. [7] The anatomy of the human eye makes desquamation of the lens impossible. [8]

Skin is the layer of usually soft, flexible outer tissue covering the body of a vertebrate animal, with three main functions: protection, regulation, and sensation.

The integumentary system is the set of organs forming the outermost layer of an animal's body. It comprises the skin and its appendages, which act as a physical barrier between the external environment and the internal environment that it serves to protect and maintain the body of the animal. Mainly it is the body's outer skin.

Keratinocytes are the primary type of cell found in the epidermis, the outermost layer of the skin. In humans, they constitute 90% of epidermal skin cells. Basal cells in the basal layer of the skin are sometimes referred to as basal keratinocytes. Keratinocytes form a barrier against environmental damage by heat, UV radiation, water loss, pathogenic bacteria, fungi, parasites, and viruses. A number of structural proteins, enzymes, lipids, and antimicrobial peptides contribute to maintain the important barrier function of the skin. Keratinocytes differentiate from epidermal stem cells in the lower part of the epidermis and migrate towards the surface, finally becoming corneocytes and eventually being shed, which happens every 40 to 56 days in humans.
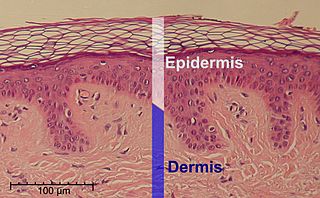
The epidermis is the outermost of the three layers that comprise the skin, the inner layers being the dermis and hypodermis. The epidermis layer provides a barrier to infection from environmental pathogens and regulates the amount of water released from the body into the atmosphere through transepidermal water loss.

The stratum corneum is the outermost layer of the epidermis. Consisting of dead tissue, it protects underlying tissue from infection, dehydration, chemicals and mechanical stress. It is composed of 15–20 layers of flattened cells with no nuclei and cell organelles.

Hyperkeratosis is thickening of the stratum corneum, often associated with the presence of an abnormal quantity of keratin, and is usually accompanied by an increase in the granular layer. As the corneum layer normally varies greatly in thickness in different sites, some experience is needed to assess minor degrees of hyperkeratosis.

The stratum granulosum is a thin layer of cells in the epidermis lying above the stratum spinosum and below the stratum corneum. Keratinocytes migrating from the underlying stratum spinosum become known as granular cells in this layer. These cells contain keratohyalin granules, which are filled with histidine- and cysteine-rich proteins that appear to bind the keratin filaments together. Therefore, the main function of keratohyalin granules is to bind intermediate keratin filaments together.
Kallikreins are a subgroup of serine proteases, enzymes capable of cleaving peptide bonds in proteins. In humans, plasma kallikrein has no known paralogue, while tissue kallikrein-related peptidases (KLKs) encode a family of fifteen closely related serine proteases. These genes are localised to chromosome 19q13, forming the largest contiguous cluster of proteases within the human genome. Kallikreins are responsible for the coordination of various physiological functions including blood pressure, semen liquefaction and skin desquamation.

A stratified squamous epithelium consists of squamous (flattened) epithelial cells arranged in layers upon a basal membrane. Only one layer is in contact with the basement membrane; the other layers adhere to one another to maintain structural integrity. Although this epithelium is referred to as squamous, many cells within the layers may not be flattened; this is due to the convention of naming epithelia according to the cell type at the surface. In the deeper layers, the cells may be columnar or cuboidal. There are no intercellular spaces. This type of epithelium is well suited to areas in the body subject to constant abrasion, as the thickest layers can be sequentially sloughed off and replaced before the basement membrane is exposed. It forms the outermost layer of the skin and the inner lining of the mouth, esophagus and vagina.

In cell biology, lamellar bodies are secretory organelles found in type II alveolar cells in the lungs, and in keratinocytes in the skin. They are oblong structures, appearing about 300-400 nm in width and 100-150 nm in length in transmission electron microscopy images. Lamellar bodies in the alveoli of the lungs fuse with the cell membrane and release pulmonary surfactant into the extracellular space.
Corneocytes are terminally differentiated keratinocytes and compose most of the stratum corneum, the outermost layer of the epidermis. They are regularly replaced through desquamation and renewal from lower epidermal layers and are essential for its function as a skin barrier.
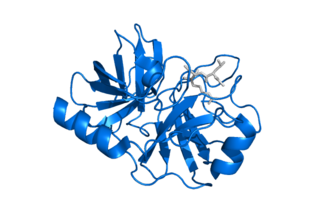
Kallikrein-5, formerly known as stratum corneum tryptic enzyme (SCTE), is a serine protease expressed in the epidermis. In humans it is encoded by the KLK5 gene. This gene is one of the fifteen kallikrein subfamily members located in a cluster on chromosome 19. Its expression is up-regulated by estrogens and progestins. Alternative splicing results in multiple transcript variants encoding the same protein.
Lympho-epithelial Kazal-type-related inhibitor (LEKTI) also known as serine protease inhibitor Kazal-type 5 (SPINK5) is a protein that in humans is encoded by the SPINK5 gene.
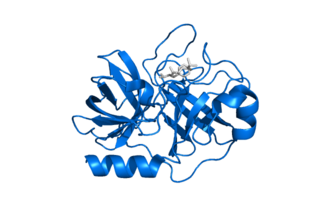
Kallikrein-related peptidase 7 (KLK7) is a serine protease that in humans is encoded by the KLK7 gene. KLK7 was initially purified from the epidermis and characterised as stratum corneum chymotryptic enzyme (SCCE). It was later identified as the seventh member of the human kallikrein family, which includes fifteen homologous serine proteases located on chromosome 19 (19q13).
Trichorrhexis invaginata is a distinctive hair shaft abnormality that may occur sporadically, either in normal hair or with other hair shaft abnormalities, or regularly as a marker for Netherton syndrome. The primary defect appears to be abnormal keratinization of the hair shaft in the keratogenous zone, allowing for intussusception of the fully keratinized and hard distal shaft into the incompletely keratinized and soft proximal portion of the shaft.

Peeling skin syndrome is an autosomal recessive disorder characterized by lifelong peeling of the stratum corneum, and may be associated with pruritus, short stature, and easily removed anagen hair.

Bullous impetigo is a bacterial skin infection caused by Staphylococcus aureus that results in the formation of large blisters called bullae, usually in areas with skin folds like the armpit, groin, between the fingers or toes, beneath the breast, and between the buttocks. It accounts for 30% of cases of impetigo, the other 70% being non-bullous impetigo.
Skin sloughing is the process of shedding dead surface cells from the skin. It is most associated with cosmetic skin maintenance via exfoliation, but can also occur biologically or for medical reasons.
TGM5 is a transglutaminase enzyme.

Lympho-epithelial Kazal-type related inhibitor 2 (LEKTI-2) is a protein encoded by the SPINK9 gene in humans. SPINK9 is a member of a gene family cluster located on chromosome 5q33.1, which includes SPINK5 and SPINK6. LEKTI-2 is an inhibitor of KLK5.