Related Research Articles
An eating disorder is a mental disorder defined by abnormal eating behaviors that negatively affect a person's physical or mental health. Types of eating disorders include binge eating disorder, where the patient eats a large amount in a short period of time; anorexia nervosa, where the person has an intense fear of gaining weight and restricts food or overexercises to manage this fear; bulimia nervosa, where individuals eat a large quantity (binging) then try to rid themselves of the food (purging); pica, where the patient eats non-food items; rumination syndrome, where the patient regurgitates undigested or minimally digested food; avoidant/restrictive food intake disorder (ARFID), where people have a reduced or selective food intake due to some psychological reasons; and a group of other specified feeding or eating disorders. Anxiety disorders, depression and substance abuse are common among people with eating disorders. These disorders do not include obesity. People often experience comorbidity between an eating disorder and OCD. It is estimated 20–60% of patients with an ED have a history of OCD.

Borderline personality disorder (BPD), also known as emotionally unstable personality disorder (EUPD), is a personality disorder characterized by a long-term pattern of intense and unstable interpersonal relationships, distorted sense of self, and strong emotional reactions. Those affected often engage in self-harm and other dangerous behaviors, often due to their difficulty with returning their emotional level to a healthy or normal baseline. They may also struggle with dissociation, a feeling of emptiness, and a fear of abandonment.

Bulimia nervosa, also known as simply bulimia, is an eating disorder characterized by binge eating followed by purging or fasting, and excessive concern with body shape and weight. This activity aims to expel the body of calories eaten from the binging phase of the process. Binge eating refers to eating a large amount of food in a short amount of time. Purging refers to the attempts to get rid of the food consumed. This may be done by vomiting or taking laxatives.
Histrionic personality disorder (HPD) is defined by the American Psychiatric Association as a personality disorder characterized by a pattern of excessive attention-seeking behaviors, usually beginning in early adulthood, including inappropriate seduction and an excessive desire for approval. People diagnosed with the disorder are said to be lively, dramatic, vivacious, enthusiastic, extroverted and flirtatious.
Orthorexia nervosa is a proposed eating disorder characterized by an excessive preoccupation with eating healthy food. The term was introduced in 1997 by American physician Steven Bratman, M.D. He suggested that some people's dietary restrictions intended to promote health may paradoxically lead to unhealthy consequences, such as social isolation; anxiety; loss of ability to eat in a natural, intuitive manner; reduced interest in the full range of other healthy human activities; and, in rare cases, severe malnutrition or even death.

Obsessive–compulsive personality disorder (OCPD) is a cluster C personality disorder marked by a spectrum of obsessions with rules, lists, schedules, and order, among other things. Symptoms are usually present by the time a person reaches adulthood, and are visible in a variety of situations. The cause of OCPD is thought to involve a combination of genetic and environmental factors, namely problems with attachment.
Binge eating disorder (BED) is an eating disorder characterized by frequent and recurrent binge eating episodes with associated negative psychological and social problems, but without the compensatory behaviors common to bulimia nervosa, OSFED, or the binge-purge subtype of anorexia nervosa.
Binge eating is a pattern of disordered eating which consists of episodes of uncontrollable eating. It is a common symptom of eating disorders such as binge eating disorder and bulimia nervosa. During such binges, a person rapidly consumes an excessive quantity of food. A diagnosis of binge eating is associated with feelings of loss of control. Binge eating disorder is also linked with being overweight and obesity.

Kleptomania is the inability to resist the urge to steal items, usually for reasons other than personal use or financial gain. First described in 1816, kleptomania is classified in psychiatry as an impulse control disorder. Some of the main characteristics of the disorder suggest that kleptomania could be an obsessive-compulsive spectrum disorder, but also share similarities with addictive and mood disorders.
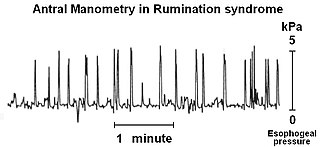
Rumination syndrome, or merycism, is a chronic motility disorder characterized by effortless regurgitation of most meals following consumption, due to the involuntary contraction of the muscles around the abdomen. There is no retching, nausea, heartburn, odour, or abdominal pain associated with the regurgitation as there is with typical vomiting, and the regurgitated food is undigested. The disorder has been historically documented as affecting only infants, young children, and people with cognitive disabilities . It is increasingly being diagnosed in a greater number of otherwise healthy adolescents and adults, though there is a lack of awareness of the condition by doctors, patients, and the general public.
The obsessive–compulsive spectrum is a model of medical classification where various psychiatric, neurological and/or medical conditions are described as existing on a spectrum of conditions related to obsessive–compulsive disorder (OCD). "The disorders are thought to lie on a spectrum from impulsive to compulsive where impulsivity is said to persist due to deficits in the ability to inhibit repetitive behavior with known negative consequences, while compulsivity persists as a consequence of deficits in recognizing completion of tasks." OCD is a mental disorder characterized by obsessions and/or compulsions. An obsession is defined as "a recurring thought, image, or urge that the individual cannot control". Compulsion can be described as a "ritualistic behavior that the person feels compelled to perform". The model suggests that many conditions overlap with OCD in symptomatic profile, demographics, family history, neurobiology, comorbidity, clinical course and response to various pharmacotherapies. Conditions described as being on the spectrum are sometimes referred to as obsessive–compulsive spectrum disorders.
The Eating Attitudes Test, created by David Garner, is a widely used 26-item, standardized self-reported questionnaire of symptoms and concerns characteristic of eating disorders. The EAT is useful in assessing "eating disorder risk" in high school, college and other special risk samples such as athletes. EAT has been extremely effective in screening for anorexia nervosa in many populations.
Avoidant/restrictive food intake disorder (ARFID) is a feeding or eating disorder in which people avoid eating certain foods, or restrict their diets to the point it ultimately results in nutritional deficiencies. This can be due to the sensory characteristics of food, such as its appearance, smell, texture, or taste; due to fear of negative consequences such as choking or vomiting; having little interest in eating or food, or a combination of these factors. People with ARFID may also be afraid of trying new foods, a fear known as food neophobia.
Diabulimia, also known as ED-DMT1 in the US or T1ED in the UK, is an eating disorder in which people with type 1 diabetes deliberately give themselves less insulin than they need or stop taking it altogether for the purpose of weight loss. Diabulimia is not recognized as a formal psychiatric diagnosis in the DSM-5. Because of this, some in the medical or psychiatric communities use the phrases "disturbed eating behavior" or "disordered eating behavior" and disordered eating (DE) are quite common in medical and psychiatric literature addressing patients who have type 1 diabetes and manipulate insulin doses to control weight along with exhibiting bulimic behavior.
Purging disorder is an eating disorder characterized by the DSM-5 as self-induced vomiting, or misuse of laxatives, diuretics, or enemas to forcefully evacuate matter from the body. Purging disorder differs from bulimia nervosa (BN) because individuals do not consume a large amount of food before they purge. In current diagnostic systems, purging disorder is a form of other specified feeding or eating disorder. Research indicates that purging disorder, while not rare, is not as commonly found as anorexia nervosa or bulimia nervosa. This syndrome is associated with clinically significant levels of distress, and that it appears to be distinct from bulimia nervosa on measures of hunger and ability to control food intake. Some of the signs of purging disorder are frequent trips to the bathroom directly after a meal, frequent use of laxatives, and obsession over one's appearance and weight. Other signs include swollen cheeks, popped blood vessels in the eyes, and clear teeth which are all signs of excessive vomiting.

Anorexia nervosa (AN), often referred to simply as anorexia, is an eating disorder characterized by food restriction, body image disturbance, fear of gaining weight, and an overpowering desire to be thin.

Depression, one of the most commonly diagnosed psychiatric disorders, is being diagnosed in increasing numbers in various segments of the population worldwide. Depression in the United States alone affects 17.6 million Americans each year or 1 in 6 people. Depressed patients are at increased risk of type 2 diabetes, cardiovascular disease and suicide. Within the next twenty years depression is expected to become the second leading cause of disability worldwide and the leading cause in high-income nations, including the United States. In approximately 75% of suicides, the individuals had seen a physician within the prior year before their death, 45–66% within the prior month. About a third of those who died by suicide had contact with mental health services in the prior year, a fifth within the preceding month.
Cognitive behavioral therapy (CBT) is derived from both the cognitive and behavioral schools of psychology and focuses on the alteration of thoughts and actions with the goal of treating various disorders. The cognitive behavioral treatment of eating disorders emphasizes on the minimization of negative thoughts about body image and the act of eating, and attempts to alter negative and harmful behaviors that are involved in and perpetuate eating disorders. It also encourages the ability to tolerate negative thoughts and feelings as well as the ability to think about food and body perception in a multi-dimensional way. The emphasis is not only placed on altering cognition, but also on tangible practices like making goals and being rewarded for meeting those goals. CBT is a "time-limited and focused approach" which means that it is important for the patients of this type of therapy to have particular issues that they want to address when they begin treatment. CBT has also proven to be one of the most effective treatments for eating disorders.
Paul E. Garfinkel is a Canadian psychiatrist, researcher and an academic leader. He is a professor at the University of Toronto and a staff psychiatrist at Centre for Addiction and Mental Health (CAMH).
Body image disturbance (BID) is a common symptom in patients with eating disorders and is characterized by an altered perception of one's own body.
References
- ↑ Marshall, J. B.; Russell, J. L. (1993). "Achalasia mistakenly diagnosed as eating disorder and prompting prolonged psychiatric hospitalization". Southern Medical Journal. 86 (12): 1405–1407. doi:10.1097/00007611-199312000-00019. PMID 8272922.
- ↑ Crisp, A. H. (1977). "The differential diagnosis of anorexia nervosa". Proceedings of the Royal Society of Medicine. 70 (10): 686–690. doi:10.1177/003591577707001004. PMC 1543424 . PMID 928375.
- ↑ Richterich, A.; Brunner, R.; Resch, F. (2003). "Achalasia mimicking prepubertal anorexia nervosa". International Journal of Eating Disorders. 33 (3): 356–359. doi:10.1002/eat.10144. PMID 12655633.
- ↑ Okada, F. (1990). "Psychiatric aspects of acute pandysautonomia". European Archives of Psychiatry and Clinical Neuroscience. 240 (2): 134–135. doi:10.1007/bf02189983. PMID 2149650. S2CID 12242055.
- ↑ Alao, A. O.; Chlebowski, S.; Chung, C. (2009). "Neuropsychiatric Systemic Lupus Erythematosus Presenting as Bipolar I Disorder with Catatonic Features". Psychosomatics. 50 (5): 543–547. doi:10.1176/appi.psy.50.5.543. PMID 19855042.
- ↑ Preventing Misdiagnosis of Women: A Guide to Physical Disorders That Have Psychiatric Symptoms (Women's Mental Health and Development) by Dr. Elizabeth Adele Klonoff and Dr. Hope Landrine. Page 87 Publisher: Sage Publications, Inc; 1 edition (November 13, 1997) Language: English ISBN 0-7619-0047-0 ISBN 978-0-7619-0047-4
- ↑ Fallon, B. A.; Nields, J. A. (1994). "Lyme disease: A neuropsychiatric illness". The American Journal of Psychiatry. 151 (11): 1571–1583. doi:10.1176/ajp.151.11.1571. PMID 7943444. S2CID 22568915.
- ↑ PPachner, A. R. (1988). "Borrelia burgdorferi in the nervous system: The new "great imitator"". Annals of the New York Academy of Sciences. 539 (1): 56–64. Bibcode:1988NYASA.539...56P. doi:10.1111/j.1749-6632.1988.tb31838.x. PMID 3190104. S2CID 7629978.
- ↑ Feddersen, B.; De La Fontaine, L.; Sass, J. O.; Lutz, J.; Abicht, A.; Klopstock, T.; Verma, I. C.; Meisenzahl, E.; Pogarell, O. (2009). "Mitochondrial Neurogastrointestinal Encephalomyopathy Mimicking Anorexia Nervosa". American Journal of Psychiatry. 166 (4): 494–495. doi:10.1176/appi.ajp.2008.08101525. PMID 19339372.
- ↑ Mitochondrial Neurogastrointestinal Encephalomyopathy Mimicking Anorexia Nervosa Article Archived 2011-06-11 at the Wayback Machine
- ↑ Mitochondrial Neurogastrointestinal Encephalopathy Disease
- ↑ Gerasimidis, T.; George, F. (2009). "Superior Mesenteric Artery Syndrome". Digestive Surgery. 26 (3): 213–214. doi: 10.1159/000219330 . PMID 19468230.
- ↑ Kornmehl, P.; Weizman, Z.; Liss, Z.; Bar-Ziv, J.; Joseph, A. (1988). "Superior mesenteric artery syndrome presenting as an anorexia nervosa-like illness". Journal of Adolescent Health. 9 (4): 340–343. doi:10.1016/0197-0070(88)90263-x. PMID 3417512.
- ↑ Adams, R.; Hinkebein, M. K.; McQuillen, M.; Sutherland, S.; El Asyouty, S.; Lippmann, S. (1998). "Prompt differentiation of Addison's disease from anorexia nervosa during weight loss and vomiting". Southern Medical Journal. 91 (2): 208–211. doi:10.1097/00007611-199802000-00017. PMID 9496878. S2CID 33433769.
- ↑ Lin, L.; Liao, S. C.; Lee, Y. J.; Tseng, M. C.; Lee, M. B. (2003). "Brain tumor presenting as anorexia nervosa in a 19-year-old man". Journal of the Formosan Medical Association = Taiwan Yi Zhi. 102 (10): 737–740. PMID 14691602.
- ↑ Sokol, M. S.; Fujimoto, C. K.; Jackson, T. K.; Silberberg, P. J. (2006). "Anorexia nervosa and brain tumor in a 14-year-old girl". CNS Spectrums. 11 (9): 669–673, quiz 673. doi:10.1017/S1092852900014759. PMID 16946691. S2CID 24555337.
- ↑ Großmann, D.; Burtzlaff, C.; Griefahn, B.; Stenger, R. -D.; Wiersbitzky, H.; Wagner, W.; Lauffer, H. (2002). "Kavernom der Medulla oblongata unter dem Bild einer "Anorexia nervosa"". Klinische Pädiatrie. 214 (1): 41–44. doi:10.1055/s-2002-19864. PMID 11823953.
- ↑ Pavesi, G.; Berlucchi, S.; Feletti, A.; Opocher, G.; Scienza, R. (2006). "Hemangioblastoma of the obex mimicking anorexia nervosa". Neurology. 67 (1): 178–179. doi:10.1212/01.wnl.0000223354.86636.ed. PMID 16832109. S2CID 24386601.
- ↑ Hotta M.; et al. (1999). "A Young Man With a Hypothalimic Tumor Mimicking Anorexia Nervosa". Journal of Tokyo Women's Medical University. 69 (6): 289–295. ISSN 0040-9022. Accession number;99A0720003 Journal Code:G0684A
- ↑ Conrad, R.; Wegener, I.; Geiser, F.; Imbierowicz, K.; Liedtke, R. (2008). "Nature against nurture: Calcification in the right thalamus in a young man with anorexia nervosa and obsessive-compulsive personality disorder". CNS Spectrums. 13 (10): 906–910. doi:10.1017/S1092852900017016. PMID 18955946. S2CID 13013352.
- ↑ López-Villegas, D.; Kulisevsky, J.; Deus, J.; Junqué, C.; Pujol, J.; Guardia, E.; Grau, J. M. (1996). "Neuropsychological alterations in patients with computed tomography-detected basal ganglia calcification". Archives of Neurology. 53 (3): 251–256. doi:10.1001/archneur.1996.00550030061023. PMID 8651878.
- ↑ Wolańczyk, T.; Komender, J.; Brzozowska, A. (1997). "Catatonic syndrome preceded by symptoms of anorexia nervosa in a 14-year-old boy with arachnoid cyst". European Child & Adolescent Psychiatry. 6 (3): 166–169. doi:10.1007/bf00538989. PMID 9383651. S2CID 13598800.
- ↑ Da Silva, J.; Alves, A.; Talina, M.; Carreiro, S.; Guimarães, J. O.; Xavier, M. (2007). "Arachnoid cyst in a patient with psychosis: Case report". Annals of General Psychiatry. 6: 16. doi: 10.1186/1744-859X-6-16 . PMC 1933420 . PMID 17598903.
- ↑ Leffler, D. A.; Dennis, M.; Edwards George, J. B.; Kelly, C. P. (2007). "The interaction between eating disorders and celiac disease: An exploration of 10 cases". European Journal of Gastroenterology & Hepatology. 19 (3): 251–255. doi:10.1097/MEG.0b013e328012db37. PMID 17301653. S2CID 28264239.
- ↑ Leffler, D. A.; Dennis, M.; Edwards George, J. B.; Kelly, C. P. (2007). "The interaction between eating disorders and celiac disease: An exploration of 10 cases". European Journal of Gastroenterology & Hepatology. 19 (3): 251–255. doi:10.1097/MEG.0b013e328012db37. PMID 17301653. S2CID 28264239.
- ↑ William P. Smedley, M.D., F.A.C.S.
- ↑ Madani, T. A. (2002). "Colonic tuberculosis clinically misdiagnosed as anorexia nervosa, and radiologically and histopathologically as Crohn's disease". The Canadian Journal of Infectious Diseases. 13 (2): 136–140. doi: 10.1155/2002/879365 . PMC 2094857 . PMID 18159383.
- ↑ Blanchet, C.; Luton, J. P. (2002). "Anorexia nervosa and Crohn disease: Diagnostic intricacies and difficulties. 3 cases". Presse Médicale. 31 (7): 312–315. PMID 11899685.
- ↑ Holaday, M.; Smith, K. E.; Robertson, S.; Dallas, J. (1994). "An atypical eating disorder with Crohn's disease in a fifteen-year-old male: A case study". Adolescence. 29 (116): 865–873. PMID 7892797.
- ↑ Wellmann, W.; Pries, K.; Freyberger, H. (2008). "Die Kombination von Morbus Crohn und Anorexia-nervosa-Symptomatik". Deutsche Medizinische Wochenschrift. 106 (45): 1499–1502. doi:10.1055/s-2008-1070542. PMID 7307984.
- ↑ Rickards, H.; Prendergast, M.; Booth, I. W. (1994). "Psychiatric presentation of Crohn's disease. Diagnostic delay and increased morbidity". The British Journal of Psychiatry. 164 (2): 256–261. doi:10.1192/bjp.164.2.256. PMID 8173832. S2CID 21761490.
- ↑ Mannucci, E.; Ricca, V.; Filetti, S.; Boldrini, M.; Rotella, C. M. (2003). "Eating behavior and thyroid disease in female obese patients". Eating Behaviors. 4 (2): 173–179. doi:10.1016/S1471-0153(03)00012-6. PMID 15000980.
- ↑ Byerley, B.; Black, D. W.; Grosser, B. I. (1983). "Anorexia nervosa with hyperthyroidism: Case report". The Journal of Clinical Psychiatry. 44 (8): 308–309. PMID 6874653.
- ↑ Krahn, D. (1990). "Thyrotoxicosis and Bulimia Nervosa". Psychosomatics. 31 (2): 222–224. doi:10.1016/S0033-3182(90)72201-3. PMID 2330406.
- ↑ Tiller, J.; MacRae, A.; Schmidt, U.; Bloom, S.; Treasure, J. (1994). "The prevalence of eating disorders in thyroid disease: A pilot study". Journal of Psychosomatic Research. 38 (6): 609–616. doi:10.1016/0022-3999(94)90058-2. PMID 7990069.
- ↑ Fonseca, V.; Wakeling, A.; Havard, C. W. (1990). "Hyperthyroidism and eating disorders". BMJ (Clinical Research Ed.). 301 (6747): 322–323. doi:10.1136/bmj.301.6747.322. PMC 1663651 . PMID 2393739.
- ↑ Birmingham, C. L.; Gritzner, S.; Gutierrez, E. (2006). "Hyperthyroidism in anorexia nervosa: Case report and review of the literature". International Journal of Eating Disorders. 39 (7): 619–620. doi:10.1002/eat.20308. PMID 16958126.
- ↑ Mattingly, D.; Bhanji, S. (1995). "Hypoglycaemia and anorexia nervosa". Journal of the Royal Society of Medicine. 88 (4): 191–195. PMC 1295161 . PMID 7745563.
- ↑ Ozawa, Y.; Koyano, H.; Akama, T. (1999). "Complete recovery from intractable bulimia nervosa by the surgical cure of primary hyperparathyroidism". International Journal of Eating Disorders. 26 (1): 107–110. doi:10.1002/(SICI)1098-108X(199907)26:1<107::AID-EAT15>3.0.CO;2-U. PMID 10349592.
- ↑ Grant, C. (2005). "Insulinoma". Best Practice & Research Clinical Gastroenterology. 19 (5): 783–798. doi:10.1016/j.bpg.2005.05.008. PMID 16253900.
- ↑ Shanmugam, V.; Zimnowodzki, S.; Curtin, J.; Gorelick, P. B. (1997). "Hypoglycemic hemiplegia: Insulinoma masquerading as stroke". Journal of Stroke and Cerebrovascular Diseases. 6 (5): 368–369. doi:10.1016/s1052-3057(97)80220-0. PMID 17895035.
- ↑ Morgan, J. R. (1989). "A case of Down's syndrome, insulinoma and anorexia". Journal of Mental Deficiency Research. 33 (2): 185–187. doi:10.1111/j.1365-2788.1989.tb01465.x. PMID 2542562.
- ↑ Olsen, D. B.; Abraham, J. H. (1999). "Neuropsychiatric disorders in insulinoma". Ugeskrift for Laeger. 161 (10): 1420–1421. PMID 10085751.
- ↑ Vig, S.; Lewis, M.; Foster, K. J.; Stacey-Clear, A. (2001). "Lessons to be learned: A case study approach insulinoma presenting as a change in personality". The Journal of the Royal Society for the Promotion of Health. 121 (1): 56–61. doi:10.1177/146642400112100112. PMID 11329699. S2CID 21795209.
- ↑ Dick, B.; Schreiber, W.; Schu, U.; Shiratori, K.; Krieg, J. C. (2002). "Encephalomyelitis disseminata: A rare, but challenging differential diagnosis of anorectic disorder". The World Journal of Biological Psychiatry. 3 (4): 225–228. doi:10.3109/15622970209150626. PMID 12516315. S2CID 30337294.
- ↑ Rosenvinge, J. H.; Martinussen, M.; Ostensen, E. (2000). "The comorbidity of eating disorders and personality disorders: A meta-analytic review of studies published between 1983 and 1998". Eating and Weight Disorders. 5 (2): 52–61. doi:10.1007/bf03327480. PMID 10941603. S2CID 34981309.
- ↑ Kaye, W. H.; Bulik, C. M.; Thornton, L.; Barbarich, N.; Masters, K. (2004). "Comorbidity of Anxiety Disorders with Anorexia and Bulimia Nervosa". American Journal of Psychiatry. 161 (12): 2215–2221. doi:10.1176/appi.ajp.161.12.2215. PMID 15569892.
- ↑ Thornton, C.; Russell, J. (1997). "Obsessive compulsive comorbidity in the dieting disorders". International Journal of Eating Disorders. 21 (1): 83–87. doi:10.1002/(SICI)1098-108X(199701)21:1<83::AID-EAT10>3.0.CO;2-P. PMID 8986521.
- ↑ Vitousek, K.; Manke, F. (1994). "Personality variables and disorders in anorexia nervosa and bulimia nervosa". Journal of Abnormal Psychology. 103 (1): 137–147. doi:10.1037/0021-843X.103.1.137. PMID 8040475.
- ↑ Braun, D. L.; Sunday, S. R.; Halmi, K. A. (1994). "Psychiatric comorbidity in patients with eating disorders". Psychological Medicine. 24 (4): 859–867. doi:10.1017/S0033291700028956. PMID 7892354. S2CID 34017953.
- ↑ Spindler, A.; Milos, G. (2007). "Links between eating disorder symptom severity and psychiatric comorbidity". Eating Behaviors. 8 (3): 364–373. doi:10.1016/j.eatbeh.2006.11.012. PMID 17606234.
- ↑ Grant, J. E.; Kim, S. W.; Eckert, E. D. (2002). "Body dysmorphic disorder in patients with anorexia nervosa: Prevalence, clinical features, and delusionality of body image". International Journal of Eating Disorders. 32 (3): 291–300. doi:10.1002/eat.10091. PMID 12210643.
- ↑ Gabbay, V.; Asnis, G. M.; Bello, J. A.; Alonso, C. M.; Serras, S. J.; O'Dowd, M. A. (2003). "New onset of body dysmorphic disorder following frontotemporal lesion". Neurology. 61 (1): 123–125. doi:10.1212/01.WNL.0000069607.30528.D5. PMID 12847173. S2CID 6059843.
- ↑ Phillips, K. A.; McElroy, S. L.; Keck Jr, P. E.; Hudson, J. I.; Pope Jr, H. G. (1994). "A comparison of delusional and nondelusional body dysmorphic disorder in 100 cases". Psychopharmacology Bulletin. 30 (2): 179–186. PMID 7831453.
- ↑ Feusner, J. D.; Townsend, J.; Bystritsky, A.; Bookheimer, S. (2007). "Visual Information Processing of Faces in Body Dysmorphic Disorder". Archives of General Psychiatry. 64 (12): 1417–1425. doi:10.1001/archpsyc.64.12.1417. PMID 18056550.
- ↑ Feusner, J. D.; Yaryura-Tobias, J.; Saxena, S. (2008). "The pathophysiology of body dysmorphic disorder". Body Image. 5 (1): 3–12. doi:10.1016/j.bodyim.2007.11.002. PMC 3836287 . PMID 18314401.
- ↑ Lipsitz, J. D.; Fyer, A. J.; Paterniti, A.; Klein, D. F. (2001). "Emetophobia: Preliminary results of an internet survey". Depression and Anxiety. 14 (2): 149–152. doi: 10.1002/da.1058 . PMID 11668669. S2CID 11784677.
- ↑ Boschen, M. J. (2007). "Reconceptualizing emetophobia: A cognitive–behavioral formulation and research agenda". Journal of Anxiety Disorders. 21 (3): 407–419. doi:10.1016/j.janxdis.2006.06.007. PMID 16890398.
- ↑ Nicholls, Dasha (1999). "Eating Disorders in Children and Adolescents". Advances in Psychiatric Treatment. 5 (4): 241–249. doi: 10.1192/apt.5.4.241 .
- ↑ Shapiro, J.; Franko, D. L.; Gagne, A. (1997). "Phagophobia: A form of psychogenic dysphagia. A new entity". The Annals of Otology, Rhinology, and Laryngology. 106 (4): 286–290. doi:10.1177/000348949710600404. PMID 9109717. S2CID 22215557.
- ↑ Okada, A.; Tsukamoto, C.; Hosogi, M.; Yamanaka, E.; Watanabe, K.; Ootyou, K.; Morishima, T. (2007). "A study of psycho-pathology and treatment of children with phagophobia". Acta Medica Okayama. 61 (5): 261–269. PMID 17971843.
- ↑ De Lucas-Taracena, M. T.; Montañés-Rada, F. (2006). "Swallowing phobia: Symptoms, diagnosis and treatment". Actas Españolas de Psiquiatría. 34 (5): 309–316. PMID 16991019.
- ↑ Casper, R. C. (1998). "Depression and eating disorders". Depression and Anxiety. 8 (S1): 96–104. doi: 10.1002/(SICI)1520-6394(1998)8:1+<96::AID-DA15>3.0.CO;2-4 . PMID 9809221. S2CID 36772859.
- ↑ Serpell, L.; Livingstone, A.; Neiderman, M.; Lask, B. (2002). "Anorexia nervosa: Obsessive-compulsive disorder, obsessive-compulsive personality disorder, or neither?". Clinical Psychology Review. 22 (5): 647–669. doi:10.1016/S0272-7358(01)00112-X. PMID 12113200.
- ↑ Bulik, C. M.; Klump, K. L.; Thornton, L.; Kaplan, A. S.; Devlin, B.; Fichter, M. M.; Halmi, K. A.; Strober, M.; Woodside, D. B. (2004). "Alcohol use disorder comorbidity in eating disorders: A multicenter study". The Journal of Clinical Psychiatry. 65 (7): 1000–1006. doi:10.4088/JCP.v65n0718. PMID 15291691.
- ↑ Larsson, J. O.; Hellzén, M. (2004). "Patterns of personality disorders in women with chronic eating disorders". Eating and Weight Disorders. 9 (3): 200–205. doi:10.1007/bf03325067. PMID 15656014. S2CID 29679535.
- ↑ Swinbourne, J. M.; Touyz, S. W. (2007). "The co-morbidity of eating disorders and anxiety disorders: A review". European Eating Disorders Review. 15 (4): 253–274. doi: 10.1002/erv.784 . PMID 17676696.
- ↑ Ronningstam, E. (1996). "Pathological narcissism and narcissistic personality disorder in Axis I disorders". Harvard Review of Psychiatry. 3 (6): 326–340. doi:10.3109/10673229609017201. PMID 9384963. S2CID 21472356.
- ↑ Anderluh, M. B.; Tchanturia, K.; Rabe-Hesketh, S.; Treasure, J. (2003). "Childhood obsessive-compulsive personality traits in adult women with eating disorders: Defining a broader eating disorder phenotype". The American Journal of Psychiatry. 160 (2): 242–247. doi:10.1176/appi.ajp.160.2.242. PMID 12562569.
- ↑ Pinto, A.; Mancebo, M. C.; Eisen, J. L.; Pagano, M. E.; Rasmussen, S. A. (2006). "The Brown Longitudinal Obsessive Compulsive Study: Clinical features and symptoms of the sample at intake". The Journal of Clinical Psychiatry. 67 (5): 703–711. doi:10.4088/JCP.v67n0503. PMC 3272757 . PMID 16841619.
- ↑ Lucka, I.; Cebella, A. (2004). "Characteristics of the forming personality in children suffering from anorexia nervosa". Psychiatria Polska. 38 (6): 1011–1018. PMID 15779665.
- ↑ Anderluh, M. B.; Tchanturia, K.; Rabe-Hesketh, S.; Treasure, J. (2003). "Childhood obsessive-compulsive personality traits in adult women with eating disorders: Defining a broader eating disorder phenotype". The American Journal of Psychiatry. 160 (2): 242–247. doi:10.1176/appi.ajp.160.2.242. PMID 12562569.
- ↑ Pinto, A.; Mancebo, M. C.; Eisen, J. L.; Pagano, M. E.; Rasmussen, S. A. (2006). "The Brown Longitudinal Obsessive Compulsive Study: Clinical features and symptoms of the sample at intake". The Journal of Clinical Psychiatry. 67 (5): 703–711. doi:10.4088/JCP.v67n0503. PMC 3272757 . PMID 16841619.
- ↑ Lucka, I.; Cebella, A. (2004). "Characteristics of the forming personality in children with anorexia nervosa". Psychiatria Polska. 38 (6): 1011–1018. PMID 15779665.
- ↑ Dukarm, C. P. (2005). "Bulimia Nervosa and Attention Deficit Hyperactivity Disorder: A Possible Role for Stimulant Medication". Journal of Women's Health. 14 (4): 345–350. doi:10.1089/jwh.2005.14.345. PMID 15916509.
- ↑ Mikami, A. Y.; Hinshaw, S. P.; Arnold, L. E.; Hoza, B.; Hechtman, L.; Newcorn, J. H.; Abikoff, H. B. (2009). "Bulimia nervosa symptoms in the Multimodal Treatment Study of Children with ADHD". International Journal of Eating Disorders. 43 (3): 248–259. doi:10.1002/eat.20692. PMID 19378318.
- ↑ Biederman, J.; Ball, S. W.; Monuteaux, M. C.; Surman, C. B.; Johnson, J. L.; Zeitlin, S. (2007). "Are Girls with ADHD at Risk for Eating Disorders? Results from a Controlled, Five-Year Prospective Study". Journal of Developmental & Behavioral Pediatrics. 28 (4): 302–307. doi:10.1097/DBP.0b013e3180327917. PMID 17700082. S2CID 31596462.
- ↑ Cortese, S.; Bernardina, B. D.; Mouren, M. C. (2007). "Attention-deficit/hyperactivity disorder (ADHD) and binge eating". Nutrition Reviews. 65 (9): 404–411. doi: 10.1111/j.1753-4887.2007.tb00318.x . PMID 17958207.
- ↑ Bruce, K. R.; Steiger, H.; Koerner, N. M.; Israel, M.; Young, S. N. (2004). "Bulimia nervosa with co-morbid avoidant personality disorder: Behavioural characteristics and serotonergic function". Psychological Medicine. 34 (1): 113–124. doi:10.1017/S003329170300864X. PMID 14971632. S2CID 41886088.
- ↑ Zucker, N. L.; Losh, M.; Bulik, C. M.; Labar, K. S.; Piven, J.; Pelphrey, K. A. (2007). "Anorexia nervosa and autism spectrum disorders: Guided investigation of social cognitive endophenotypes". Psychological Bulletin. 133 (6): 976–1006. CiteSeerX 10.1.1.545.1664 . doi:10.1037/0033-2909.133.6.976. PMID 17967091.