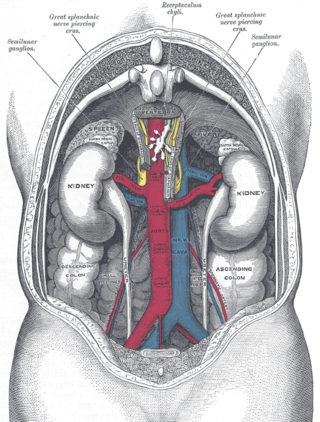
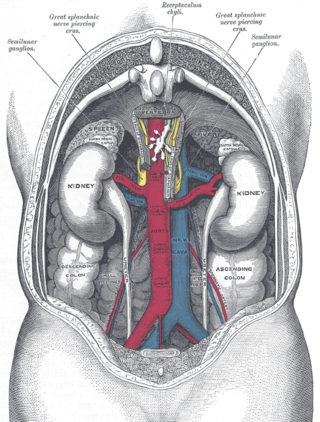
In humans, the kidneys are two reddish-brown bean-shaped blood-filtering organs that are a multilobar, multipapillary form of mammalian kidneys, usually without signs of external lobulation. They are located on the left and right in the retroperitoneal space, and in adult humans are about 12 centimetres in length. They receive blood from the paired renal arteries; blood exits into the paired renal veins. Each kidney is attached to a ureter, a tube that carries excreted urine to the bladder.

Kidney stone disease, also known as renal calculus disease, nephrolithiasis or urolithiasis, is a crystallopathy where a solid piece of material develops in the urinary tract. Renal calculi typically form in the kidney and leave the body in the urine stream. A small calculus may pass without causing symptoms. If a stone grows to more than 5 millimeters, it can cause blockage of the ureter, resulting in sharp and severe pain in the lower back or abdomen. A calculus may also result in blood in the urine, vomiting, or painful urination. About half of people who have had a renal calculus are likely to have another within ten years.

Prune belly syndrome is a rare, genetic birth defect affecting about 1 in 40,000 births. About 97% of those affected are male. Prune belly syndrome is a congenital disorder of the urinary system, characterized by a triad of symptoms. The syndrome is named for the mass of wrinkled skin that is often present on the abdomen of those with the disorder.
The excretory system is a passive biological system that removes excess, unnecessary materials from the body fluids of an organism, so as to help maintain internal chemical homeostasis and prevent damage to the body. The dual function of excretory systems is the elimination of the waste products of metabolism and to drain the body of used up and broken down components in a liquid and gaseous state. In humans and other amniotes, most of these substances leave the body as urine and to some degree exhalation, mammals also expel them through sweating.

The ureters are tubes made of smooth muscle that propel urine from the kidneys to the urinary bladder. In a human adult, the ureters are usually 20–30 cm (8–12 in) long and around 3–4 mm (0.12–0.16 in) in diameter. The ureter is lined by urothelial cells, a type of transitional epithelium, and has an additional smooth muscle layer that assists with peristalsis in its lowest third.

The renal calyces are conduits in the kidney through which urine passes. The minor calyces form a cup-shaped drain around the apex of the renal pyramids. Urine formed in the kidney passes through a renal papilla at the apex into the minor calyx; 4-5 minor calyces converge to form a major calyx through which urine passes into the renal pelvis.

A ureterocele is a congenital abnormality found in the ureter. In this condition the distal ureter balloons at its opening into the bladder, forming a sac-like pouch. It is most often associated with a duplicated collection system, where two ureters drain their respective kidney instead of one. Simple ureterocele, where the condition involves only a single ureter, represents only twenty percent of cases.

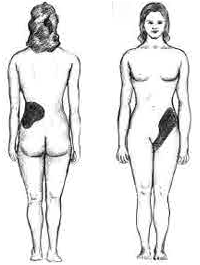
Pyelonephritis is inflammation of the kidney, typically due to a bacterial infection. Symptoms most often include fever and flank tenderness. Other symptoms may include nausea, burning with urination, and frequent urination. Complications may include pus around the kidney, sepsis, or kidney failure.

The renal arteries are paired arteries that supply the kidneys with blood. Each is directed across the crus of the diaphragm, so as to form nearly a right angle.

Hydronephrosis describes hydrostatic dilation of the renal pelvis and calyces as a result of obstruction to urine flow downstream. Alternatively, hydroureter describes the dilation of the ureter, and hydronephroureter describes the dilation of the entire upper urinary tract.
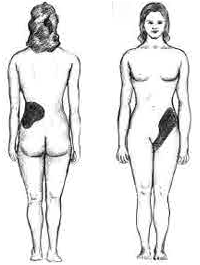
Renal colic, also known as ureteric colic, is a type of abdominal pain commonly caused by obstruction of ureter from dislodged kidney stones. The most frequent site of obstruction is the vesico-ureteric junction (VUJ), the narrowest point of the upper urinary tract. Acute obstruction and the resultant urinary stasis can distend the ureter (hydroureter) and cause a reflexive peristaltic smooth muscle spasm, which leads to a very intense visceral pain transmitted via the ureteric plexus.

Vesicoureteral reflux (VUR), also known as vesicoureteric reflux, is a condition in which urine flows retrograde, or backward, from the bladder into one or both ureters and then to the renal calyx or kidneys. Urine normally travels in one direction from the kidneys to the bladder via the ureters, with a one-way valve at the vesicoureteral (ureteral-bladder) junction preventing backflow. The valve is formed by oblique tunneling of the distal ureter through the wall of the bladder, creating a short length of ureter (1–2 cm) that can be compressed as the bladder fills. Reflux occurs if the ureter enters the bladder without sufficient tunneling, i.e., too "end-on".
Pyelogram is a form of imaging of the renal pelvis and ureter.
Ovarian vein syndrome is a rare condition in which a dilated ovarian vein compresses the ureter. This causes chronic or colicky abdominal pain, back pain and/or pelvic pain. The pain can worsen on lying down or between ovulation and menstruation. There can also be an increased tendency towards urinary tract infection or pyelonephritis. The right ovarian vein is most commonly involved, although the disease can be left-sided or affect both sides. It is currently classified as a form of pelvic congestion syndrome.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
Bladder outlet obstruction occurs when urine is unable to flow from the kidneys through the ureters and out of the bladder through the urethra. Decreased flow of urine leads to swelling of the urinary tract, called hydronephrosis. This process of decreased flow of urine through the urinary tract can begin as early as during intrauterine life and it prevents normal development of fetal kidneys and fetal urine. Low levels of fetal urine leads to low amniotic fluid levels and incomplete lung maturation. Older children and adults can also experience bladder outlet obstruction; however, this process is usually reversible and isn't associated with as many poor outcomes as in infants with congenital bladder outlet obstruction.

Fraley syndrome is a condition where the superior infundibulum of the upper calyx of the kidney is obstructed by the crossing renal artery branch, causing distension and dilatation of the calyx and presenting clinically as haematuria and nephralgia. Furthermore, when the renal artery obstructs the proximal collecting system, filling defects can occur anywhere in the calyces, pelvis, or ureter.

Ureteral cancer is cancer of the ureters, muscular tubes that propel urine from the kidneys to the urinary bladder. It is also known as ureter cancer, renal pelvic cancer, and rarely ureteric cancer or uretal cancer. Cancer in this location is rare. Ureteral cancer becomes more likely in older adults, usually ages 70–80, who have previously been diagnosed with bladder cancer.

Renal ultrasonography is the examination of one or both kidneys using medical ultrasound.
Ureteric stricture (ureteral stricture) is the pathological narrowing of the ureter which may lead to serious complications such as kidney failure.