Related Research Articles

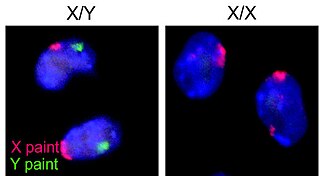
Turner syndrome (TS), also known as 45,X, or 45,X0, is a genetic disorder caused by a sex chromosome monosomy, compared to the two sex chromosomes in most people. Signs and symptoms vary among those affected. Often, a short and webbed neck, low-set ears, low hairline at the back of the neck, short stature, and swollen hands and feet are seen at birth. Typically, those affected do not develop menstrual periods or breasts without hormone treatment and are unable to have children without reproductive technology. Heart defects, diabetes, and low thyroid hormone occur in the disorder more frequently than average. Most people with Turner syndrome have normal intelligence; however, many have problems with spatial visualization that may be needed in order to learn mathematics. Vision and hearing problems also occur more often than average.
In medicine, precocious puberty is puberty occurring at an unusually early age. In most cases, the process is normal in every aspect except the unusually early age and simply represents a variation of normal development. In a minority of children with precocious puberty, the early development is triggered by a disease such as a tumor or injury of the brain. Even when there is no disease, unusually early puberty can have adverse effects on social behavior and psychological development, can reduce adult height potential, and may shift some lifelong health risks. Central precocious puberty can be treated by suppressing the pituitary hormones that induce sex steroid production. The opposite condition is delayed puberty.
Delayed puberty is when a person lacks or has incomplete development of specific sexual characteristics past the usual age of onset of puberty. The person may have no physical or hormonal signs that puberty has begun. In the United States, girls are considered to have delayed puberty if they lack breast development by age 13 or have not started menstruating by age 15. Boys are considered to have delayed puberty if they lack enlargement of the testicles by age 14. Delayed puberty affects about 2% of adolescents.
Virilization or masculinization is the biological development of adult male characteristics in young males or females. Most of the changes of virilization are produced by androgens.
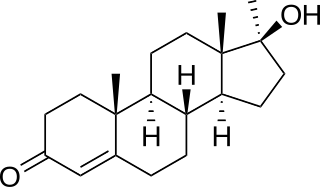
Methyltestosterone, sold under the brand names Android, Metandren, and Testred among others, is an androgen and anabolic steroid (AAS) medication which is used in the treatment of low testosterone levels in men, delayed puberty in boys, at low doses as a component of menopausal hormone therapy for menopausal symptoms like hot flashes, osteoporosis, and low sexual desire in women, and to treat breast cancer in women. It is taken by mouth or held in the cheek or under the tongue.
Adrenarche is an early stage in sexual maturation that happens in some higher primates and in humans, typically peaks at around 20 years of age, and is involved in the development of pubic hair, body odor, skin oiliness, axillary hair, sexual attraction/sexual desire/increased libido and mild acne. During adrenarche the adrenal glands secrete increased levels of weak adrenal androgens, including dehydroepiandrosterone (DHEA), dehydroepiandrosterone sulfate (DHEA-S), and androstenedione (A4), but without increased cortisol levels. Adrenarche is the result of the development of a new zone of the adrenal cortex, the zona reticularis. Adrenarche is a process related to puberty, but distinct from hypothalamic–pituitary–gonadal axis maturation and function.
Pubarche refers to the first appearance of pubic hair at puberty and also it marks the beginning of puberty. It is one of the physical changes of puberty and can occur independently of complete puberty. The early stage of sexual maturation, also known as adrenarche, is marked by characteristics including the development of pubic hair, axillary hair, adult apocrine body odor, acne, and increased oiliness of hair and skin. The Encyclopedia of Child and Adolescent Health corresponds SMR2 with pubarche, defining it as the development of pubic hair that occurs at a mean age of 11.6 years in females and 12.6 years in males. It further describes that pubarche's physical manifestation is vellus hair over the labia or the base of the penis. See Table 1 for the entirety of the Sexual Maturity Rating description.

Thelarche, also known as breast budding, is the onset of secondary breast development, often representing the beginning of pubertal development. It is the stage at which male and female breasts differentiate due to variance in hormone levels; however, some males have a condition in which they develop breasts, termed gynecomastia. Thelarche typically occurs between the ages of 8 and 13 years with significant variation between individuals. However, the initial growth of breast tissue occurs during fetal development.

Testicular atrophy is a medical condition in which one or both testicles diminish in size and may be accompanied by reduced testicular function. Testicular atrophy is not related to the temporary shrinkage of the surrounding scrotum, which might occur in response to cold temperature.

Hyperandrogenism is a medical condition characterized by high levels of androgens. It is more common in women than men. Symptoms of hyperandrogenism may include acne, seborrhea, hair loss on the scalp, increased body or facial hair, and infrequent or absent menstruation. Complications may include high blood cholesterol and diabetes. It occurs in approximately 5% of women of reproductive age.
Masculinizing hormone therapy, also known as transmasculine hormone therapy, or female-to-male hormone therapy, is a form of hormone therapy and gender affirming therapy which is used to change the secondary sexual characteristics of transgender people from feminine or androgynous to masculine. It is a common type of transgender hormone therapy, and is predominantly used to treat transgender men and other transmasculine individuals. Some intersex people also receive this form of therapy, either starting in childhood to confirm the assigned sex or later if the assignment proves to be incorrect.
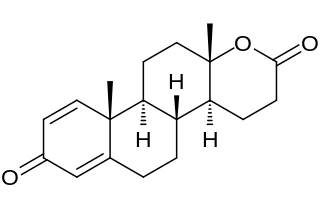
Testolactone is a non-selective, irreversible, steroidal aromatase inhibitor which is used as an antineoplastic drug to treat advanced-stage breast cancer. The drug was discontinued in 2008 and is no longer available for medical use.

Aromatase deficiency is a rare condition characterized by extremely low levels or complete absence of the enzyme aromatase activity in the body. It is an autosomal recessive disease resulting from various mutations of gene CYP19 (P450arom) which can lead to ambiguous genitalia and delayed puberty in females, continued linear growth into adulthood and osteoporosis in males and virilization in pregnant mothers. As of 2020, fewer than 15 cases have been identified in genetically male individuals and at least 30 cases in genetically female individuals.
Puberty is the process of physical changes through which a child's body matures into an adult body capable of sexual reproduction. It is initiated by hormonal signals from the brain to the gonads: the ovaries in a female, the testes in a male. In response to the signals, the gonads produce hormones that stimulate libido and the growth, function, and transformation of the brain, bones, muscle, blood, skin, hair, breasts, and sex organs. Physical growth—height and weight—accelerates in the first half of puberty and is completed when an adult body has been developed. Before puberty, the external sex organs, known as primary sexual characteristics, are sex characteristics that distinguish males and females. Puberty leads to sexual dimorphism through the development of the secondary sex characteristics, which further distinguish the sexes.

Aromatase excess syndrome is a rare genetic and endocrine syndrome which is characterized by an overexpression of aromatase, the enzyme responsible for the biosynthesis of the estrogen sex hormones from the androgens, in turn resulting in excessive levels of circulating estrogens and, accordingly, symptoms of hyperestrogenism. It affects both sexes, manifesting itself in males as marked or complete phenotypical feminization and in females as hyperfeminization.
Hypergonadotropic hypogonadism (HH), also known as primary or peripheral/gonadal hypogonadism or primary gonadal failure, is a condition which is characterized by hypogonadism which is due to an impaired response of the gonads to the gonadotropins, follicle-stimulating hormone (FSH) and luteinizing hormone (LH), and in turn a lack of sex steroid production. As compensation and the lack of negative feedback, gonadotropin levels are elevated. Individuals with HH have an intact and functioning hypothalamus and pituitary glands so they are still able to produce FSH and LH. HH may present as either congenital or acquired, but the majority of cases are of the former nature. HH can be treated with hormone replacement therapy.
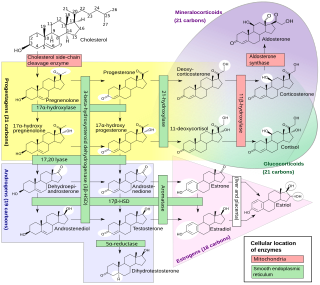
An inborn error of steroid metabolism is an inborn error of metabolism due to defects in steroid metabolism.
Hyperestrogenism, hyperestrogenic state, or estrogen excess, is a medical condition characterized by an excessive amount of estrogenic activity in the body.
Pediatric gynaecology or pediatric gynecology is the medical practice dealing with the health of the vagina, vulva, uterus, and ovaries of infants, children, and adolescents. Its counterpart is pediatric andrology, which deals with medical issues specific to the penis and testes.
The medical uses of bicalutamide, a nonsteroidal antiandrogen (NSAA), include the treatment of androgen-dependent conditions and hormone therapy to block the effects of androgens. Indications for bicalutamide include the treatment of prostate cancer in men, skin and hair conditions such as acne, seborrhea, hirsutism, and pattern hair loss in women, high testosterone levels in women, hormone therapy in transgender women, as a puberty blocker to prevent puberty in transgender girls and to treat early puberty in boys, and the treatment of long-lasting erections in men. It may also have some value in the treatment of paraphilias and hypersexuality in men.
References
- ↑ Danner HG (2014). A Thesaurus of English Word Roots. Rowman & Littlefield. p. 350. ISBN 978-1-4422-3326-3 . Retrieved 3 May 2021.
- ↑ Molina PE (2018). Endocrine physiology (Fifth ed.). New York: McGraw-Hill Education. ISBN 978-1-260-01935-3.
- ↑ "An Overview of Hypergonadism". CCCHC. 2020. Retrieved 2022-07-25.
- ↑ "Hypergonadism". hospitals.aku.edu. Retrieved 2022-07-25.