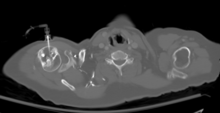
A central venous catheter (CVC), also known as a central line (c-line), central venous line, or central venous access catheter, is a catheter placed into a large vein. It is a form of venous access. Placement of larger catheters in more centrally located veins is often needed in critically ill patients, or in those requiring prolonged intravenous therapies, for more reliable vascular access. These catheters are commonly placed in veins in the neck, chest, groin, or through veins in the arms.

Intravenous therapy is a medical technique that administers fluids, medications and nutrients directly into a person's vein. The intravenous route of administration is commonly used for rehydration or to provide nutrients for those who cannot, or will not—due to reduced mental states or otherwise—consume food or water by mouth. It may also be used to administer medications or other medical therapy such as blood products or electrolytes to correct electrolyte imbalances. Attempts at providing intravenous therapy have been recorded as early as the 1400s, but the practice did not become widespread until the 1900s after the development of techniques for safe, effective use.

In pharmacology and toxicology, a route of administration is the way by which a drug, fluid, poison, or other substance is taken into the body.

Subcutaneous administration is the insertion of medications beneath the skin either by injection or infusion.

Battlefield medicine, also called field surgery and later combat casualty care, is the treatment of wounded combatants and non-combatants in or near an area of combat. Civilian medicine has been greatly advanced by procedures that were first developed to treat the wounds inflicted during combat. With the advent of advanced procedures and medical technology, even polytrauma can be survivable in modern wars. Battlefield medicine is a category of military medicine.

An injection is the act of administering a liquid, especially a drug, into a person's body using a needle and a syringe. An injection is considered a form of parenteral drug administration; it does not involve absorption in the digestive tract. This allows the medication to be absorbed more rapidly and avoid the first pass effect. There are many types of injection, which are generally named after the body tissue the injection is administered into. This includes common injections such as subcutaneous, intramuscular, and intravenous injections, as well as less common injections such as intraperitoneal, intraosseous, intracardiac, intraarticular, and intracavernous injections.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

A peripherally inserted central catheter, less commonly called a percutaneous indwelling central catheter, is a form of intravenous access that can be used for a prolonged period of time or for administration of substances that should not be done peripherally. It is a catheter that enters the body through the skin (percutaneously) at a peripheral site, extends to the superior vena cava, and stays in place for days, weeks or even months.

Advanced Life Support (ALS) is a set of life saving protocols and skills that extend basic life support to further support the circulation and provide an open airway and adequate ventilation (breathing).
Extravasation is the leakage of intravenously (IV) infused, and potentially damaging, medications into the extravascular tissue around the site of infusion. The leakage can occur through brittle veins in the elderly, through previous venipuncture access, or through direct leakage from wrongly positioned venous access devices. When the leakage is not of harmful consequence it is known as infiltration. Extravasation of medication during intravenous therapy is an adverse event related to therapy that, depending on the medication, amount of exposure, and location, can potentially cause serious injury and permanent harm, such as tissue necrosis. Milder consequences of extravasation include irritation, characterized by symptoms of pain and inflammation, with the clinical signs of warmth, erythema, or tenderness.

Intracardiac injections are injections that are given directly into the heart muscles or ventricles. They can be used in emergencies, although they are rarely used in modern practice.
Venous cutdown is an emergency procedure in which the vein is exposed surgically and then a cannula is inserted into the vein under direct vision. It is used for venous access in cases of trauma, and hypovolemic shock when the use of a peripheral venous catheter is either difficult or impossible. The great saphenous vein is most commonly used. This procedure has fallen out of favor with the development of safer techniques for central venous catheterization such as the Seldinger technique, the modified Seldinger technique, intraosseous infusion, as well as the use of ultrasound guidance for placement of central venous catheters without using the cutdown technique.

In medicine, a port is a small medical appliance that is installed beneath the skin. A catheter connects the port to a vein. Under the skin, the port has a septum through which drugs can be injected and blood samples can be drawn many times, usually with less discomfort for the patient than a more typical "needle stick".
An advanced emergency medical technician is a provider of emergency medical services in the United States. A transition to this level of training from the emergency medical technician-intermediate, which have somewhat less training, began in 2013 and has been implemented by most states. AEMTs are not intended to deliver definitive medical care in most cases, but rather to augment prehospital critical care and provide rapid on-scene treatment. AEMTs are usually employed in ambulance services, working in conjunction with EMTs and paramedics; however they are also commonly found in fire departments and law enforcement agencies as non-transporting first responders. Ambulances operating at the AEMT level of care are commonplace in rural areas, and occasionally found in larger cities as part of a tiered-response system, but are overall much less common than EMT- and paramedic-level ambulances. The AEMT provides a low-cost, high-benefit option to provide advanced-level care when the paramedic level of care is not feasible. The AEMT is authorized to provide limited advanced life support, which is beyond the scope of an EMT.
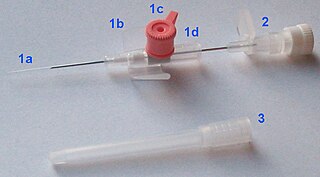
In medicine, a peripheral venous catheter, peripheral venous line, peripheral venous access catheter, or peripheral intravenous catheter, is a catheter placed into a peripheral vein for venous access to administer intravenous therapy such as medication fluids.
The Hs and Ts is a mnemonic used to aid in remembering the possible reversible causes of cardiac arrest. A variety of disease processes can lead to a cardiac arrest; however, they usually boil down to one or more of the "Hs and Ts".
ICU Medical, Inc. is a San Clemente, California-based company with global operations. ICU Medical products are designed to prevent bloodstream infections and protect healthcare workers from exposure to infectious diseases or hazardous drugs. ICU Medical product line includes intravenous therapy (IV) products, pumps, needle-free vascular access devices, custom infusion sets, closed system hazardous drug handling devices and systems, sensor catheters, needle-free closed blood sampling systems, and hemodynamic monitoring systems.
Established in 2001, Vidacare Corporation was the developer of intraosseous medical devices. Its devices were used in vascular access, emergency and disaster medicine, oncology, and spinal surgery. Privately held, the company was based in San Antonio, Texas, and its products were marketed in over 50 countries worldwide.
Venous access is any method used to access the bloodstream through the veins, either to administer intravenous therapy, parenteral nutrition, to obtain blood for analysis, or to provide an access point for blood-based treatments such as dialysis or apheresis. Access is most commonly achieved via the Seldinger technique, and guidance tools such as ultrasound and fluoroscopy can also be used to assist with visualizing access placement.

Intracerebroventricular injection is a route of administration for drugs via injection into the cerebral ventricles so that it reaches the cerebrospinal fluid (CSF). This route of administration is often used to bypass the blood-brain barrier because it can prevent important medications from reaching the central nervous system. This injection method is widely used in diseased mice models to study the effect of drugs, plasmid DNA, and viral vectors on the central nervous system. In humans, ICV injection can be used for the administration of drugs for various reasons. Examples include the treatment of Spinal Muscular Atrophy (SMA), the administration of chemotherapy in gliomas, and the administration of drugs for long-term pain management. ICV injection is also used in the creation of diseased animal models specifically to model neurological disorders.