The labia minora, also known as the inner labia, inner lips, or nymphae, are two flaps of skin that are part of the primate vulva, extending outwards from the vaginal and urethral openings to encompass the vestibule. The labia minora are situated between the labia majora and together form the labia. They vary widely in size, color and shape from individual to individual.
Vulvodynia is a chronic pain condition that affects the vulvar area and occurs without an identifiable cause. Symptoms typically include a feeling of burning or irritation. It has been established by the ISSVD that for the diagnosis to be made symptoms must last at least three months.

In human anatomy, and in mammals in general, the mons pubis or pubic mound is a rounded mass of fatty tissue found over the pubic symphysis of the pubic bones.
Vaginitis, also known as vulvovaginitis, is inflammation of the vagina and vulva. Symptoms may include itching, burning, pain, discharge, and a bad smell. Certain types of vaginitis may result in complications during pregnancy.
An imperforate hymen is a congenital disorder where a hymen without an opening completely obstructs the vagina. It is caused by a failure of the hymen to perforate during fetal development. It is most often diagnosed in adolescent girls when menstrual blood accumulates in the vagina and sometimes also in the uterus. It is treated by surgical incision of the hymen.

The labia are the major externally visible portions of the vulva. In humans and other primates, there are two pairs of labia: the labia majora are large and thick folds of skin that cover the vulva's other parts while the labia minora are the inner folds of skin between the outer labia that surround and protect the urethral and vaginal openings.
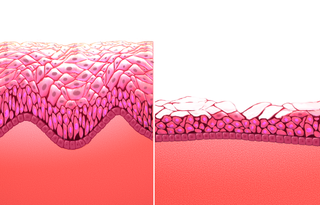
Vulvitis is inflammation of the vulva, the external female mammalian genitalia that include the labia majora, labia minora, clitoris, and introitus. It may co-occur as vulvovaginitis with vaginitis, inflammation of the vagina, and may have infectious or non-infectious causes. The warm and moist conditions of the vulva make it easily affected. Vulvitis is prone to occur in any female especially those who have certain sensitivities, infections, allergies, or diseases that make them likely to have vulvitis. Postmenopausal women and prepubescent girls are more prone to be affected by it, as compared to women in their menstruation period. It is so because they have low estrogen levels which makes their vulvar tissue thin and dry. Women having diabetes are also prone to be affected by vulvitis due to the high sugar content in their cells, increasing their vulnerability. Vulvitis is not a disease, it is just an inflammation caused by an infection, allergy or injury. Vulvitis may also be symptom of any sexually transmitted infection or a fungal infection.

Labiaplasty is a plastic surgery procedure for creating or altering the labia minora and the labia majora, the folds of skin of the human vulva. It is a type of vulvoplasty. There are two main categories of women seeking cosmetic genital surgery: those with congenital conditions such as intersex, and those with no underlying condition who experience physical discomfort or wish to alter the appearance of their vulvas because they believe they do not fall within a normal range.

Vaginal discharge is a mixture of liquid, cells, and bacteria that lubricate and protect the vagina. This mixture is constantly produced by the cells of the vagina and cervix, and it exits the body through the vaginal opening. The composition, amount, and quality of discharge varies between individuals and can vary throughout the menstrual cycle and throughout the stages of sexual and reproductive development. Normal vaginal discharge may have a thin, watery consistency or a thick, sticky consistency, and it may be clear or white in color. Normal vaginal discharge may be large in volume but typically does not have a strong odor, nor is it typically associated with itching or pain. While most discharge is considered physiologic or represents normal functioning of the body, some changes in discharge can reflect infection or other pathological processes. Infections that may cause changes in vaginal discharge include vaginal yeast infections, bacterial vaginosis, and sexually transmitted infections. The characteristics of abnormal vaginal discharge vary depending on the cause, but common features include a change in color, a foul odor, and associated symptoms such as itching, burning, pelvic pain, or pain during sexual intercourse.

Vaginectomy is a surgery to remove all or part of the vagina. It is one form of treatment for individuals with vaginal cancer or rectal cancer that is used to remove tissue with cancerous cells. It can also be used in gender-affirming surgery. Some people born with a vagina who identify as trans men or as nonbinary may choose vaginectomy in conjunction with other surgeries to make the clitoris more penis-like (metoidioplasty), construct of a full-size penis (phalloplasty), or create a relatively smooth, featureless genital area.

The vulval vestibule is the part of the vulva between the labia minora. On the inside, the urinary meatus and the vaginal opening open to the vestibule, while the outer edge is marked by Hart's line, named after David Berry Hart.

A pelvic examination is the physical examination of the external and internal female pelvic organs. It is frequently used in gynecology for the evaluation of symptoms affecting the female reproductive and urinary tract, such as pain, bleeding, discharge, urinary incontinence, or trauma. It can also be used to assess a woman's anatomy in preparation for procedures. The exam can be done awake in the clinic and emergency department, or under anesthesia in the operating room. The most commonly performed components of the exam are 1) the external exam, to evaluate the vulva 2) the internal exam with palpation to examine the uterus, ovaries, and structures adjacent to the uterus (adnexae) and 3) the internal exam using a speculum to visualize the vaginal walls and cervix. During the pelvic exam, sample of cells and fluids may be collected to screen for sexually transmitted infections or cancer.

Hematometra is a medical condition involving collection or retention of blood in the uterus. It is most commonly caused by an imperforate hymen or a transverse vaginal septum.

Multicystic dysplastic kidney (MCDK) is a condition that results from the malformation of the kidney during fetal development. The kidney consists of irregular cysts of varying sizes. Multicystic dysplastic kidney is a common type of renal cystic disease, and it is a cause of an abdominal mass in infants.
Genital leiomyomas are leiomyomas that originate in the dartos muscles, or smooth muscles, of the genitalia, areola, and nipple. They are a subtype of cutaneous leiomyomas that affect smooth muscle found in the scrotum, labia, or nipple. They are benign tumors, but may cause pain and discomfort to patients. Genital leiomyoma can be symptomatic or asymptomatic and is dependent on the type of leiomyoma. In most cases, pain in the affected area or region is most common. For vaginal leiomyoma, vaginal bleeding and pain may occur. Uterine leiomyoma may exhibit pain in the area as well as painful bowel movement and/or sexual intercourse. Nipple pain, enlargement, and tenderness can be a symptom of nipple-areolar leiomyomas. Genital leiomyomas can be caused by multiple factors, one can be genetic mutations that affect hormones such as estrogen and progesterone. Moreover, risk factors to the development of genital leiomyomas include age, race, and gender. Ultrasound and imaging procedures are used to diagnose genital leiomyomas, while surgically removing the tumor is the most common treatment of these diseases. Case studies for nipple areolar, scrotal, and uterine leiomyoma were used, since there were not enough secondary resources to provide more evidence.

Clitoral hood reduction, also termed clitoral hoodectomy, clitoral unhooding, clitoridotomy, or (partial) hoodectomy, is a plastic surgery procedure for reducing the size and the area of the clitoral hood in order to further expose the glans of the clitoris.

In mammals, the vulva consists of the external female genitalia. The human vulva includes the mons pubis, labia majora, labia minora, clitoris, vulval vestibule, urinary meatus, the vaginal opening, hymen, and Bartholin's and Skene's vestibular glands. The urinary meatus is also included as it opens into the vulval vestibule. The vulva includes the entrance to the vagina, which leads to the uterus, and provides a double layer of protection for this by the folds of the outer and inner labia. Pelvic floor muscles support the structures of the vulva. Other muscles of the urogenital triangle also give support.

The Prader scale or Prader staging, named after Andrea Prader, is a coarse rating system for the measurement of the degree of virilization of the genitalia of the human body and is similar to the Quigley scale. It primarily relates to virilization of the female genitalia in cases of congenital adrenal hyperplasia (CAH) and identifies five distinct stages, but in recent times has been used to describe the range of differentiation of genitalia, with normal infant presentation being shown on either end of the scale, female on the left (0) and male on the right (6).
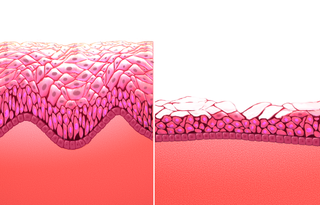
Atrophic vaginitis is inflammation of the vagina as a result of tissue thinning due to not enough estrogen. Symptoms may include pain with sex, vaginal itchiness or dryness, and an urge to urinate or burning with urination. It generally does not resolve without ongoing treatment. Complications may include urinary tract infections.
Pediatric gynaecology or pediatric gynecology is the medical practice dealing with the health of the vagina, vulva, uterus, and ovaries of infants, children, and adolescents. Its counterpart is pediatric andrology, which deals with medical issues specific to the penis and testes.