A teratoma is a tumor made up of several different types of tissue, such as hair, muscle, teeth, or bone. Teratomata typically form in the tailbone, ovary, or testicle.

Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle or swelling or pain in the scrotum. Treatment may result in infertility.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

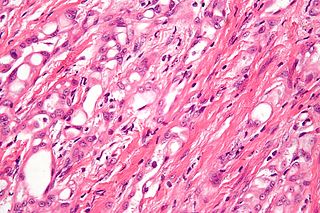
Leydig cells, also known as interstitial cells of the testes and interstitial cells of Leydig, are found adjacent to the seminiferous tubules in the testicle and produce testosterone in the presence of luteinizing hormone (LH). They are polyhedral in shape and have a large, prominent nucleus, an eosinophilic cytoplasm, and numerous lipid-filled vesicles.

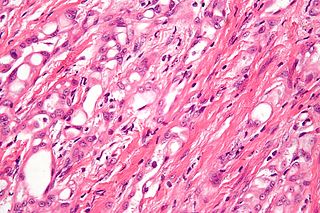
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal neoplasms of the gastrointestinal tract. GISTs arise in the smooth muscle pacemaker interstitial cell of Cajal, or similar cells. They are defined as tumors whose behavior is driven by mutations in the KIT gene (85%), PDGFRA gene (10%), or BRAF kinase (rare). 95% of GISTs stain positively for KIT (CD117). Most (66%) occur in the stomach and gastric GISTs have a lower malignant potential than tumors found elsewhere in the GI tract.

Brenner tumours are an uncommon subtype of the surface epithelial-stromal tumour group of ovarian neoplasms. The majority are benign, but some can be malignant.

Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in this group are thought to be derived from the ovarian surface epithelium or from ectopic endometrial or Fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This group of tumors accounts for 90% to 95% of all cases of ovarian cancer; however is mainly only found in postmenopausal women with the exception of the United States where 7% of cases occur in women under the age of 40. Serum CA-125 is often elevated but is only 50% accurate so it is not a useful tumor marker to assess the progress of treatment. 75% of women with epithelial ovarian cancer are found within the advanced-stages; however younger patients are more likely to have better prognoses than older patients.
Sertoli–Leydig cell tumour is a group of tumors composed of variable proportions of Sertoli cells, Leydig cells, and in the case of intermediate and poorly differentiated neoplasms, primitive gonadal stroma and sometimes heterologous elements.

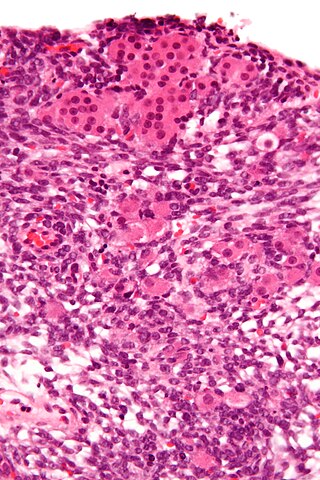
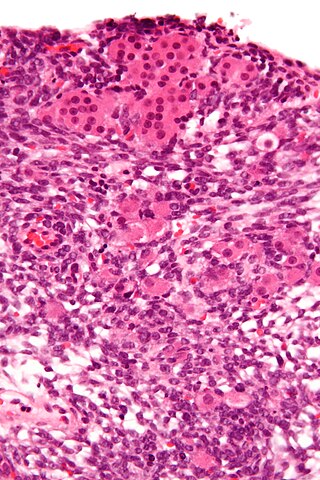
Granulosa cell tumours are tumours that arise from granulosa cells. They are estrogen secreting tumours and present as large, complex, ovarian masses. These tumours are part of the sex cord–gonadal stromal tumour or non-epithelial group of tumours. Although granulosa cells normally occur only in the ovary, granulosa cell tumours occur in both ovaries and testicles. These tumours should be considered malignant and treated in the same way as other malignant tumours of ovary. The ovarian disease has two forms, juvenile and adult, both characterized by indolent growth, and therefore has high recovery rates. The staging system for these tumours is the same as for epithelial tumours and most present as stage I. The peak age at which they occur is 50–55 years, but they may occur at any age.

Sex cord–gonadal stromal tumour is a group of tumors derived from the stromal component of the ovary and testis, which comprises the granulosa, thecal cells and fibrocytes. In contrast, the epithelial cells originate from the outer epithelial lining surrounding the gonad while the germ cell tumors arise from the precursor cells of the gametes, hence the name germ cell. In humans, this group accounts for 8% of ovarian cancers and under 5% of testicular cancers. Their diagnosis is histological: only a biopsy of the tumour can make an exact diagnosis. They are often suspected of being malignant prior to operation, being solid ovarian tumours that tend to occur most commonly in post menopausal women.

Germ cell tumor (GCT) is a neoplasm derived from germ cells. Germ-cell tumors can be cancerous or benign. Germ cells normally occur inside the gonads. GCTs that originate outside the gonads may be birth defects resulting from errors during development of the embryo.

A seminoma is a germ cell tumor of the testicle or, more rarely, the mediastinum or other extra-gonadal locations. It is a malignant neoplasm and is one of the most treatable and curable cancers, with a survival rate above 95% if discovered in early stages.

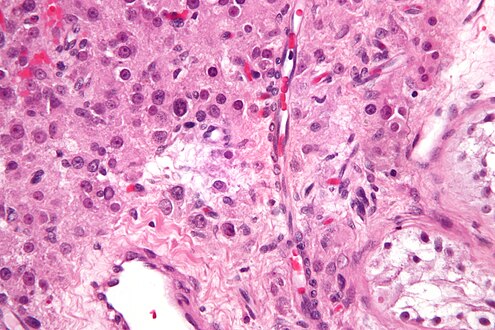
Embryonal carcinoma is a relatively uncommon type of germ cell tumour that occurs in the ovaries and testes.
Adenomatoid tumors are rare and benign mesothelial tumors, which arise from the lining of organs. It mainly presents in the genital tract, in regions such as the testis and epididymis. Because of this, researchers had a difficult time concluding that type of tumor has a mesothelial origin. Immunohistochemisty staining of tumor samples show that it is indeed positive for mesothelial-markers. It is the most common extratesticular neoplasm after lipoma, and accounts for 30% of these masses. On the other hand, adenomatoid tumors are the most common tumors of testicular adnexa. Although they are more common to be found in the paratesticular region they are sometimes found in the intratesticular region. It also has been found in other organs such as the pancreas, liver, mesocolon, and adrenal glands. In the female, it has been found in the body of the uterus and the fallopian tube. Most adenomatoid tumors do not cause much pain and can go unnoticed for a long time. Of course, there are a few exceptions to this absence of pain. An example of this is when adenomatoid tumors grow too close to testicular adnexal structures. Tumors of this kind are usually found to be asymptomatic and easily treatable.

Germ cell neoplasia in situ (GCNIS) represents the precursor lesion for many types of testicular germ cell tumors.
Sarcoidosis is a systemic disease of unknown cause that results in the formation of non-caseating granulomas in multiple organs. The prevalence is higher among black males than white males by a ratio of 20:1. Usually the disease is localized to the chest, but urogenital involvement is found in 0.2% of clinically diagnosed cases and 5% of those diagnosed at necropsy. The kidney is the most frequently affected urogenital organ, followed in men by the epididymis. Testicular sarcoidosis can present as a diffuse painless scrotal mass or can mimic acute epididymo-orchitis. Usually it appears with systemic manifestations of the disease. Since it causes occlusion and fibrosis of the ductus epididymis, fertility may be affected. On ultrasound, the hypoechogenicity and ‘infiltrative’ pattern seen in the present case are recognized features. Opinions differ on the need for histological proof, with reports of limited biopsy and frozen section, radical orchiectomy in unilateral disease and unilateral orchiectomy in bilateral disease. The peak incidence of sarcoidosis and testicular neoplasia coincide at 20–40 years and this is why most patients end up having an orchiectomy. However, testicular tumours are much more common in white men, less than 3.5% of all testicular tumours being found in black men. These racial variations justify a more conservative approach in patients of Afro-Caribbean descent with proven sarcoidosis elsewhere. Careful follow-up and ultrasonic surveillance may be preferable in certain clinical settings to biopsy and surgery, especially in patients with bilateral testicular disease.

A Sertoli cell tumour, also Sertoli cell tumor, is a sex cord–gonadal stromal tumour of Sertoli cells. They can occur in the testis or ovary. They are very rare and generally peak between the ages of 35 and 50. They are typically well-differentiated, and may be misdiagnosed as seminomas as they often appear very similar.

Orchiectomy is a surgical procedure in which one or both testicles are removed. The surgery is performed as treatment for testicular cancer, as part of surgery for transgender women, as management for advanced prostate cancer, and to remove damaged testes after testicular torsion. Less frequently, orchiectomy may be performed following a trauma, or due to wasting away of one or more testicles.

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
Reinke crystals are rod-like cytoplasmic inclusions which can be found in Leydig cells of the testes. Occurring only in adult humans and wild bush rats, their function is unknown.