Amputation is the removal of a limb by trauma, medical illness, or surgery. As a surgical measure, it is used to control pain or a disease process in the affected limb, such as malignancy or gangrene. In some cases, it is carried out on individuals as a preventive surgery for such problems. A special case is that of congenital amputation, a congenital disorder, where fetal limbs have been cut off by constrictive bands. In some countries, amputation is currently used to punish people who commit crimes. Amputation has also been used as a tactic in war and acts of terrorism; it may also occur as a war injury. In some cultures and religions, minor amputations or mutilations are considered a ritual accomplishment. When done by a person, the person executing the amputation is an amputator. The oldest evidence of this practice comes from a skeleton found buried in Liang Tebo cave, East Kalimantan, Indonesian Borneo dating back to at least 31,000 years ago, where it was done when the amputee was a young child.

In medicine, a prosthesis, or a prosthetic implant, is an artificial device that replaces a missing body part, which may be lost through trauma, disease, or a condition present at birth. Prostheses are intended to restore the normal functions of the missing body part. Amputee rehabilitation is primarily coordinated by a physiatrist as part of an inter-disciplinary team consisting of physiatrists, prosthetists, nurses, physical therapists, and occupational therapists. Prostheses can be created by hand or with computer-aided design (CAD), a software interface that helps creators design and analyze the creation with computer-generated 2-D and 3-D graphics as well as analysis and optimization tools.

Orthopedic surgery or orthopedics is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors, and congenital disorders.

Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant, that is, a hip prosthesis. Hip replacement surgery can be performed as a total replacement or a hemi/semi(half) replacement. Such joint replacement orthopaedic surgery is generally conducted to relieve arthritis pain or in some hip fractures. A total hip replacement consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is one of the most common orthopaedic operations, though patient satisfaction varies widely. Approximately 58% of total hip replacements are estimated to last 25 years. The average cost of a total hip replacement in 2012 was $40,364 in the United States, and about $7,700 to $12,000 in most European countries.

Bone grafting is a surgical procedure that replaces missing bone in order to repair bone fractures that are extremely complex, pose a significant health risk to the patient, or fail to heal properly. Some small or acute fractures can be cured without bone grafting, but the risk is greater for large fractures like compound fractures.

Arthrodesis, also known as artificial ankylosis or syndesis, is the artificial induction of joint ossification between two bones by surgery. This is done to relieve intractable pain in a joint which cannot be managed by pain medication, splints, or other normally indicated treatments. The typical causes of such pain are fractures which disrupt the joint, severe sprains, and arthritis. It is most commonly performed on joints in the spine, hand, ankle, and foot. Historically, knee and hip arthrodeses were also performed as pain-relieving procedures, but with the great successes achieved in hip and knee arthroplasty, arthrodesis of these large joints has fallen out of favour as a primary procedure, and now is only used as a procedure of last resort in some failed arthroplasties.
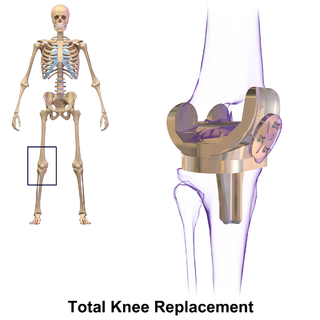
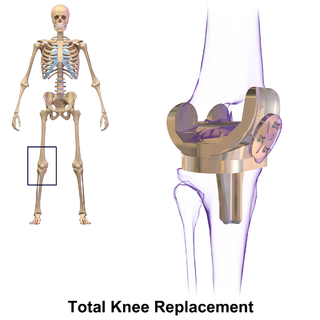
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources. It may also be performed for other knee diseases, such as rheumatoid arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation, and is not a reason to perform knee replacement.

Computer-assisted orthopedic surgery or computer-assisted orthopaedic surgery is a discipline where computer technology is applied pre-, intra- and/or post-operatively to improve the outcome of orthopedic surgical procedures. Although records show that it has been implemented since the 1990s, CAOS is still an active research discipline which brings together orthopedic practitioners with traditionally technical disciplines, such as engineering, computer science and robotics.

Joint replacement is a procedure of orthopedic surgery known also as arthroplasty, in which an arthritic or dysfunctional joint surface is replaced with an orthopedic prosthesis. Joint replacement is considered as a treatment when severe joint pain or dysfunction is not alleviated by less-invasive therapies. Joint replacement surgery is often indicated from various joint diseases, including osteoarthritis and rheumatoid arthritis.
Rotationplasty, commonly known as a Van Nes rotation or Borggreve rotation, is a type of autograft wherein a portion of a limb is removed, while the remaining limb below the involved portion is rotated and reattached. This procedure is used when a portion of an extremity is injured or involved with a disease, such as cancer.
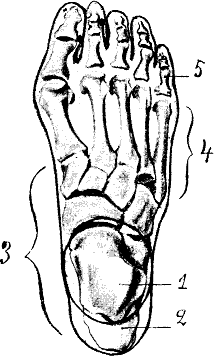
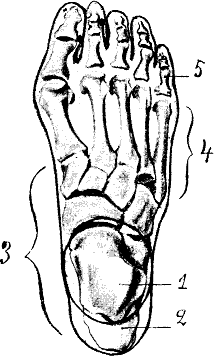
Hallux rigidus or stiff big toe is degenerative arthritis and stiffness due to bone spurs that affects the metatarsophalangeal joints (MTP) at the base of the hallux.

Shoulder replacement is a surgical procedure in which all or part of the glenohumeral joint is replaced by a prosthetic implant. Such joint replacement surgery generally is conducted to relieve arthritis pain or fix severe physical joint damage.
Epiphysiodesis is a pediatric orthopedic surgery procedure that aims at altering or stopping the bone growth naturally occurring through the growth plate also known as the physeal plate. There are two types of epiphysiodesis: temporary hemiepiphysiodesis and permanent epiphysiodesis. Temporary hemiepiphysiodesis is also known as guided growth surgery or growth modulation surgery. Temporary hemiepiphysiodesis is reversible i.e. the metal implants used to achieve epiphysiodesis can be removed after the desired correction is achieved and the growth plate can thus resume its normal growth and function. In contrast, permanent epiphysiodesis is irreversible and the growth plate function cannot be restored after surgery. Both temporary hemiepiphysiodesis and permanent epiphysiodesis are used to treat a diverse array of pediatric orthopedic disorders but the exact indications for each procedure are different.
Ankle replacement, or ankle arthroplasty, is a surgical procedure to replace the damaged articular surfaces of the human ankle joint with prosthetic components. This procedure is becoming the treatment of choice for patients requiring arthroplasty, replacing the conventional use of arthrodesis, i.e. fusion of the bones. The restoration of range of motion is the key feature in favor of ankle replacement with respect to arthrodesis. However, clinical evidence of the superiority of the former has only been demonstrated for particular isolated implant designs.
"Professor" Derek McMinn is a British orthopaedic surgeon and inventor who practised in Birmingham, United Kingdom at the BMI Edgbaston Hospital until his suspension in 2020. McMinn is currently under police investigation for allegedly keeping the body parts of thousands of patients over a 25-year period.
The following outline is provided as an overview of and topical guide to trauma and orthopaedics:

Orthopedic surgery is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal injuries, sports injuries, degenerative diseases, infections, bone tumours, and congenital limb deformities. Trauma surgery and traumatology is a sub-specialty dealing with the operative management of fractures, major trauma and the multiply-injured patient.

Reverse shoulder replacement is a type of shoulder replacement in which the normal ball and socket relationship of glenohumeral joint is reversed, creating a more stable joint with a fixed fulcrum. This form of shoulder replacement is utilized in situations in which conventional shoulder replacement surgery would lead to poor outcomes and high failure rates.
Ankle fusion, or ankle arthrodesis, is surgery of the ankle to fuse the bones to treat arthritis and for other purposes. There are different types of ankle fusion surgery. The surgery involves the use of screws, plates, medical nails, and other hardware to achieve bone union. Ankle fusion is considered to be the gold standard for treatment of end-stage ankle arthritis. It trades joint mobility for relief from pain. Complications may include infection, non-union, and, rarely, amputation.