Related Research Articles
Albuminuria is a pathological condition wherein the protein albumin is abnormally present in the urine. It is a type of proteinuria. Albumin is a major plasma protein ; in healthy people, only trace amounts of it are present in urine, whereas larger amounts occur in the urine of patients with kidney disease. For a number of reasons, clinical terminology is changing to focus on albuminuria more than proteinuria.

Creatinine is a breakdown product of creatine phosphate from muscle and protein metabolism. It is released at a constant rate by the body.

Proteinuria is the presence of excess proteins in the urine. In healthy persons, urine contains very little protein, less than 150 mg/day; an excess is suggestive of illness. Excess protein in the urine often causes the urine to become foamy. Severe proteinuria can cause nephrotic syndrome in which there is worsening swelling of the body.

Kidney failure, also known as end-stage renal disease (ESRD), is a medical condition in which the kidneys can no longer adequately filter waste products from the blood, functioning at less than 15% of normal levels. Kidney failure is classified as either acute kidney failure, which develops rapidly and may resolve; and chronic kidney failure, which develops slowly and can often be irreversible. Symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications of acute and chronic failure include uremia, hyperkalemia, and volume overload. Complications of chronic failure also include heart disease, high blood pressure, and anaemia.

Renal functions include maintaining an acid–base balance; regulating fluid balance; regulating sodium, potassium, and other electrolytes; clearing toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

Assessment of kidney function occurs in different ways, using the presence of symptoms and signs, as well as measurements using urine tests, blood tests, and medical imaging.

Kidney disease, or renal disease, technically referred to as nephropathy, is damage to or disease of a kidney. Nephritis is an inflammatory kidney disease and has several types according to the location of the inflammation. Inflammation can be diagnosed by blood tests. Nephrosis is non-inflammatory kidney disease. Nephritis and nephrosis can give rise to nephritic syndrome and nephrotic syndrome respectively. Kidney disease usually causes a loss of kidney function to some degree and can result in kidney failure, the complete loss of kidney function. Kidney failure is known as the end-stage of kidney disease, where dialysis or a kidney transplant is the only treatment option.

Chronic kidney disease (CKD) is a type of kidney disease in which a gradual loss of kidney function occurs over a period of months to years. Initially generally no symptoms are seen, but later symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications can relate to hormonal dysfunction of the kidneys and include high blood pressure, bone disease, and anemia. Additionally CKD patients have markedly increased cardiovascular complications with increased risks of death and hospitalization.

Diabetic nephropathy, also known as diabetic kidney disease, is the chronic loss of kidney function occurring in those with diabetes mellitus. Diabetic nephropathy is the leading causes of chronic kidney disease (CKD) and end-stage renal disease (ESRD) globally. The triad of protein leaking into the urine, rising blood pressure with hypertension and then falling renal function is common to many forms of CKD. Protein loss in the urine due to damage of the glomeruli may become massive, and cause a low serum albumin with resulting generalized body swelling (edema) so called nephrotic syndrome. Likewise, the estimated glomerular filtration rate (eGFR) may progressively fall from a normal of over 90 ml/min/1.73m2 to less than 15, at which point the patient is said to have end-stage renal disease. It usually is slowly progressive over years.

Hypertensive kidney disease is a medical condition referring to damage to the kidney due to chronic high blood pressure. It manifests as hypertensive nephrosclerosis. It should be distinguished from renovascular hypertension, which is a form of secondary hypertension, and thus has opposite direction of causation.
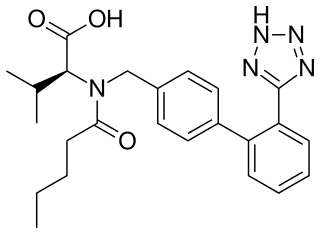
Valsartan, sold under the brand name Diovan among others, is a medication used to treat high blood pressure, heart failure, and diabetic kidney disease. It belongs to a class of medications referred to as angiotensin II receptor blockers (ARBs). It is a reasonable initial treatment for high blood pressure. It is taken by mouth.
Contrast-induced nephropathy (CIN) is a purported form of kidney damage in which there has been recent exposure to medical imaging contrast material without another clear cause for the acute kidney injury.
Fructosamines are compounds that result from glycation reactions between a sugar and a primary amine, followed by isomerization via the Amadori rearrangement. Biologically, fructosamines are recognized by fructosamine-3-kinase, which may trigger the degradation of advanced glycation end-products. Fructosamine can also refer to the specific compound 1-amino-1-deoxy-D-fructose (isoglucosamine), first synthesized by Nobel laureate Hermann Emil Fischer in 1886.
Phosphate nephropathy or nephrocalcinosis is an adverse renal condition that arises with a formation of phosphate crystals within the kidney's tubules. This renal insufficiency is associated with the use of oral sodium phosphate (OSP) such as C.B. Fleet's Phospho soda and Salix's Visocol, for bowel cleansing prior to a colonoscopy.
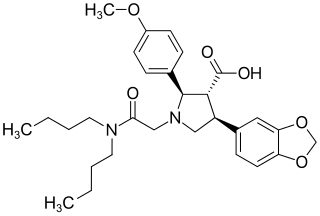
Atrasentan is an experimental drug that is being studied for the treatment of various types of cancer, including non-small cell lung cancer. It is also being investigated as a therapy for diabetic kidney disease.
Sickle cell nephropathy is a type of nephropathy associated with sickle cell disease which causes kidney complications as a result of sickling of red blood cells in the small blood vessels. The hypertonic and relatively hypoxic environment of the renal medulla, coupled with the slow blood flow in the vasa recta, favors sickling of red blood cells, with resultant local infarction. Functional tubule defects in patients with sickle cell disease are likely the result of partial ischemic injury to the renal tubules.

1,5-Anhydroglucitol, also known as 1,5-AG, is a naturally occurring monosaccharide found in nearly all foods. Blood concentrations of 1,5-anhydroglucitol decrease during times of hyperglycemia above 180 mg/dL, and return to normal levels after approximately 2 weeks in the absence of hyperglycemia. As a result, it can be used for people with either type-1 or type-2 diabetes mellitus to identify glycemic variability or a history of high blood glucose even if current glycemic measurements such as hemoglobin A1c (HbA1c) and blood glucose monitoring have near normal values. Despite this possible use and its approval by the FDA, 1,5-AG tests are rarely ordered. There is some data suggesting that 1,5-AG values are useful to fill the gap and offer complementary information to HbA1c and fructosamine tests.

Orthostatic albuminuria, also known as orthostatic proteinuria is defined by raised levels of urine protein excretion while in an upright position. In orthostatic albuminuria urine protein excretion returns to normal while in a supine position, such as laying down. Orthostatic albuminuria is the most common cause of isolated proteinuria in those under 20. The prevalence of orthostatic albuminuria is suspected to be between 2 and 5%, however some studies suggest that it is more common. Orthostatic albuminuria is diagnosed if urine protein levels are normal in a morning urine sample and there are no other obvious causes of albuminuria. Patients with orthostatic albuminuria are often asymptomatic and there is no indication for any type of treatment or interventions.

Glomerular hyperfiltration is a situation where the filtration elements in the kidneys called glomeruli produce excessive amounts of pro-urine. It can be part of a number of medical conditions particularly diabetic nephropathy.

Finerenone, sold under the brand name Kerendia and Firialta, is a medication used to reduce the risk of kidney function decline, kidney failure, cardiovascular death, non-fatal heart attacks, and hospitalization for heart failure in adults with chronic kidney disease associated with type 2 diabetes. Finerenone is a non-steroidal mineralocorticoid receptor antagonist (MRA). It is taken orally.
References
- Abid O, Sun Q, Sugimoto K, Mercan D, Vincent JL (2001). "Predictive value of microalbuminuria in medical ICU patients: results of a pilot study". Chest. 120 (6): 1984–8. doi:10.1378/chest.120.6.1984. PMID 11742932.
- Andersen S, Blouch K, Bialek J, Deckert M, Parving HH, Myers BD (2000). "Glomerular permselectivity in early stages of overt diabetic nephropathy". Kidney Int. 58 (5): 2129–37. doi: 10.1111/j.1523-1755.2000.00386.x . PMID 11044234.
- Heart Outcomes Prevention Evaluation Study Investigators (2000). "Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy". Lancet. 355 (9200): 253–9. doi:10.1016/S0140-6736(99)12323-7. PMID 10675071. S2CID 1863533.
- Lemley KV, Abdullah I, Myers BD, et al. (2000). "Evolution of incipient nephropathy in type 2 diabetes mellitus". Kidney Int. 58 (3): 1228–37. doi: 10.1046/j.1523-1755.2000.00223.x . PMID 10972685.
- Lièvre M, Marre M, Chatellier G, et al. (2000). "The non-insulin-dependent diabetes, hypertension, microalbuminuria or proteinuria, cardiovascular events, and ramipril (DIABHYCAR) study: design, organization, and patient recruitment. DIABHYCAR Study Group". Controlled Clinical Trials . 21 (4): 383–96. doi:10.1016/S0197-2456(00)00060-X. PMID 10913814.
- Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P (2001). "The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes". N. Engl. J. Med. 345 (12): 870–8. doi: 10.1056/NEJMoa011489 . PMID 11565519.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney inter., Suppl. 2013; 3: 1–150.