Related Research Articles

Acetazolamide, sold under the trade name Diamox among others, is a medication used to treat glaucoma, epilepsy, altitude sickness, periodic paralysis, idiopathic intracranial hypertension, and heart failure. It may be used long term for the treatment of open angle glaucoma and short term for acute angle closure glaucoma until surgery can be carried out. It is taken by mouth or injection into a vein.
Alkalosis is the result of a process increase hydrogen ion concentration of arterial blood plasma (alkalemia). In contrast to acidemia, alkalemia occurs when the serum pH is higher than normal. Alkalosis is usually divided into the categories of respiratory alkalosis and metabolic alkalosis or a combined respiratory/metabolic alkalosis.

Renal physiology is the study of the physiology of the kidney. This encompasses all functions of the kidney, including maintenance of acid-base balance; regulation of fluid balance; regulation of sodium, potassium, and other electrolytes; clearance of toxins; absorption of glucose, amino acids, and other small molecules; regulation of blood pressure; production of various hormones, such as erythropoietin; and activation of vitamin D.

Hyperkalemia is an elevated level of potassium (K+) in the blood. Normal potassium levels are between 3.5 and 5.0 mmol/L (3.5 and 5.0 mEq/L) with levels above 5.5 mmol/L defined as hyperkalemia. Typically hyperkalemia does not cause symptoms. Occasionally when severe it can cause palpitations, muscle pain, muscle weakness, or numbness. Hyperkalemia can cause an abnormal heart rhythm which can result in cardiac arrest and death.
Hyperchloremia is an electrolyte disturbance in which there is an elevated level of the chloride ions in the blood. The normal serum range for chloride is 96 to 106 mEq/L, therefore chloride levels at or above 110 mEq/L usually indicate kidney dysfunction as it is a regulator of chloride concentration. As of now there are no specific symptoms of hyperchloremia, however, it can be the influenced by multiple abnormalities that cause a loss of electrolyte-free fluid, loss of hypotonic fluid, or increased administration of sodium chloride. These abnormalities are caused by diarrhea, vomiting, increased sodium chloride intake, renal dysfunction, diuretic use, and diabetes. Hyperchloremia should not be mistaken for hyperchloremic metabolic acidosis as hyperchloremic metabolic acidosis is characterized by two major changes: a decrease in blood pH and bicarbonate levels, as well as an increase in blood chloride levels. Instead those with hyperchloremic metabolic acidosis are usually predisposed to hyperchloremia.

Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids. Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35. Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low, normal, to high.
The anion gap is a value calculated from the results of multiple individual medical lab tests. It may be reported with the results of an electrolyte panel, which is often performed as part of a comprehensive metabolic panel.

Metabolic alkalosis is a metabolic condition in which the pH of tissue is elevated beyond the normal range (7.35–7.45). This is the result of decreased hydrogen ion concentration, leading to increased bicarbonate, or alternatively a direct result of increased bicarbonate concentrations. The condition typically cannot last long if the kidneys are functioning properly.
Band 3 anion transport protein, also known as anion exchanger 1 (AE1) or band 3 or solute carrier family 4 member 1 (SLC4A1), is a protein that is encoded by the SLC4A1 gene in humans.
In physiology, base excess and base deficit refer to an excess or deficit, respectively, in the amount of base present in the blood. The value is usually reported as a concentration in units of mEq/L (mmol/L), with positive numbers indicating an excess of base and negative a deficit. A typical reference range for base excess is −2 to +2 mEq/L.
Hyperchloremic acidosis is a form of metabolic acidosis associated with a normal anion gap, a decrease in plasma bicarbonate concentration, and an increase in plasma chloride concentration. Although plasma anion gap is normal, this condition is often associated with an increased urine anion gap, due to the kidney's inability to secrete ammonia.

Renal tubular acidosis (RTA) is a medical condition that involves an accumulation of acid in the body due to a failure of the kidneys to appropriately acidify the urine. In renal physiology, when blood is filtered by the kidney, the filtrate passes through the tubules of the nephron, allowing for exchange of salts, acid equivalents, and other solutes before it drains into the bladder as urine. The metabolic acidosis that results from RTA may be caused either by failure to reabsorb sufficient bicarbonate ions from the filtrate in the early portion of the nephron or by insufficient secretion of hydrogen ions into the latter portions of the nephron. Although a metabolic acidosis also occurs in those with chronic kidney disease, the term RTA is reserved for individuals with poor urinary acidification in otherwise well-functioning kidneys. Several different types of RTA exist, which all have different syndromes and different causes. RTA is usually an incidental finding based on routine blood draws that show abnormal results. Clinically, patients may present with vague symptoms such as dehydration, mental status changes, or delayed growth in adolescents.
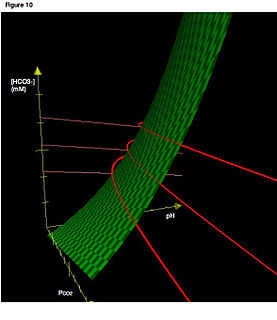
Acid–base homeostasis is the homeostatic regulation of the pH of the body's extracellular fluid (ECF). The proper balance between the acids and bases in the ECF is crucial for the normal physiology of the body, and cellular metabolism. The pH of the intracellular fluid and the extracellular fluid need to be maintained at a constant level.
Normal anion gap acidosis is an acidosis that is not accompanied by an abnormally increased anion gap.
Acid–base imbalance is an abnormality of the human body's normal balance of acids and bases that causes the plasma pH to deviate out of the normal range. In the fetus, the normal range differs based on which umbilical vessel is sampled. It can exist in varying levels of severity, some life-threatening.
Lightwood–Albright syndrome is a neonatal form of renal tubular acidosis. It is characterized by distal renal tubular acidosis that occurs as a result of bicarbonate wasting and the inability to excrete hydrogen ions. By definition, it is a transient process and has no particular disease course. If untreated, it may lead to nephrocalcinosis and failure to thrive.

High anion gap metabolic acidosis is a form of metabolic acidosis characterized by a high anion gap. Metabolic acidosis occurs when the body produces too much acid, or when the kidneys are not removing enough acid from the body. Several types of metabolic acidosis occur, grouped by their influence on the anion gap. The anion gap can be increased due to relatively low levels of cations other than sodium and potassium. An anion gap is usually considered to be high if it is over 12 mEq/L.

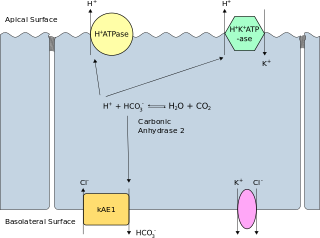
Distal renal tubular acidosis (dRTA) is the classical form of RTA, being the first described. Distal RTA is characterized by a failure of acid secretion by the alpha intercalated cells of the cortical collecting duct of the distal nephron. This failure of acid secretion may be due to a number of causes, and it leads to an inability to acidify the urine to a pH of less than 5.3.
Proximal renal tubular acidosis (pRTA) or type 2 renal tubular acidosis (RTA) is a type of RTA caused by a failure of the proximal tubular cells to reabsorb filtered bicarbonate from the urine, leading to urinary bicarbonate wasting and subsequent acidemia. The distal intercalated cells function normally, so the acidemia is less severe than dRTA and the urine can acidify to a pH of less than 5.3. pRTA also has several causes, and may occasionally be present as a solitary defect, but is usually associated with a more generalised dysfunction of the proximal tubular cells called Fanconi syndrome where there is also phosphaturia, glycosuria, aminoaciduria, uricosuria and tubular proteinuria.
Delta ratio, or "delta-delta", is a formula that can be used to assess elevated anion gap metabolic acidosis and to evaluate whether a mixed acid-base disorder is present. The anion gap (AG) without potassium is calculated first and if a metabolic acidosis is present, results in either a high anion gap metabolic acidosis (HAGMA) or a normal anion gap acidosis (NAGMA). A low anion gap is usually an oddity of measurement, rather than a clinical concern.
References
- ↑ Kim GH, Han JS, Kim YS, Joo KW, Kim S, Lee JS (January 1996). "Evaluation of urine acidification by urine anion gap and urine osmolal gap in chronic metabolic acidosis". Am. J. Kidney Dis. 27 (1): 42–7. doi:10.1016/S0272-6386(96)90029-3. PMID 8546137.
- ↑ "Urine Anion Gap: Acid Base Tutorial, University of Connecticut Health Center". Archived from the original on 2008-11-21. Retrieved 2009-04-11.
- ↑ Julia A. McMillan; Ralph D. Feigin; Catherine DeAngelis; M. Douglas Jones (1 April 2006). Oski's pediatrics: principles & practice. Lippincott Williams & Wilkins. pp. 1–. ISBN 978-0-7817-3894-1 . Retrieved 14 November 2010.
- ↑ Batlle DC, Hizon M, Cohen E, Gutterman C, Gupta R. The use of the urinary anion gap in the diagnosis of hyperchloremic metabolic acidosis. N Engl J Med. 1988;318(10):594-9.
- ↑ Goldstein, MB; Bear, R; Richardson, RM; Marsden, PA; Halperin, ML (Oct 1986). "The urine anion gap: a clinically useful index of ammonium excretion". The American Journal of the Medical Sciences. 292 (4): 198–202. doi:10.1097/00000441-198610000-00003. PMID 3752165.