Related Research Articles

Dandruff is a skin condition that mainly affects the scalp. Symptoms include flaking and sometimes mild itchiness. It can result in social or self-esteem problems. A more severe form of the condition, which includes inflammation of the skin, is known as seborrhoeic dermatitis.

Irritant diaper dermatitis is a generic term applied to skin rash in the diaper area that are caused by various skin disorders and/or irritants.

The stratum corneum is the outermost layer of the epidermis. Consisting of dead tissue, it protects underlying tissue from infection, dehydration, chemicals and mechanical stress. It is composed of 15–20 layers of flattened cells with no nuclei and cell organelles.

Desquamation, or peeling skin, is the shedding of dead cells from the outermost layer of skin.

Filaggrin is a filament-associated protein that binds to keratin fibers in epithelial cells. Ten to twelve filaggrin units are post-translationally hydrolyzed from a large profilaggrin precursor protein during terminal differentiation of epidermal cells. In humans, profilaggrin is encoded by the FLG gene, which is part of the S100 fused-type protein (SFTP) family within the epidermal differentiation complex on chromosome 1q21. In cetaceans and sirenians, the FLG family has lost its function, with the curious exception of manatees in the latter clade: manatees still retain some functional FLG genes.

Urocanic acid is an intermediate in the catabolism of L-histidine. The cis-urocanic acid isomer is rare.

Louis-Anne-Jean Brocq was a French dermatologist born in Laroque-Timbaut, a village in the department of Lot-et-Garonne.
Corneocytes are terminally differentiated keratinocytes and compose most of the stratum corneum, the outermost layer of the epidermis. They are regularly replaced through desquamation and renewal from lower epidermal layers and are essential for its function as a skin barrier.
Kallikrein-related peptidase 7 (KLK7) is a serine protease that in humans is encoded by the KLK7 gene. KLK7 was initially purified from the epidermis and characterised as stratum corneum chymotryptic enzyme (SCCE). It was later identified as the seventh member of the human kallikrein family, which includes fifteen homologous serine proteases located on chromosome 19 (19q13).

Dermatitis herpetiformis (DH) is a chronic autoimmune blistering skin condition, characterised by intensely itchy blisters filled with a watery fluid. DH is a cutaneous manifestation of coeliac disease, although the exact causal mechanism is not known. DH is neither related to nor caused by herpes virus; the name means that it is a skin inflammation having an appearance similar to herpes.

Parakeratosis is a mode of keratinization characterized by the retention of nuclei in the stratum corneum. In mucous membranes, parakeratosis is normal. In the skin, this process leads to the abnormal replacement of annular squames with nucleated cells. Parakeratosis is associated with the thinning or loss of the granular layer and is usually seen in diseases of increased cell turnover, whether inflammatory or neoplastic. Parakeratosis is seen in the plaques of psoriasis and in dandruff.
Impetigo herpetiformis is a form of severe pustular psoriasis occurring in pregnancy which may occur during any trimester.
Inverse psoriasis or flexural psoriasis is a form of psoriasis that selectively, and often exclusively, involves the folds, recesses, and flexor surfaces such as the ears, axillae, groin folds, inframammary folds, navel, intergluteal cleft, penis, and lips.

Bullous impetigo is a bacterial skin infection caused by Staphylococcus aureus that results in the formation of large blisters called bullae, usually in areas with skin folds like the armpit, groin, between the fingers or toes, beneath the breast, and between the buttocks. It accounts for 30% of cases of impetigo, the other 70% being non-bullous impetigo.
Skin sloughing is the process of shedding dead surface cells from the skin. It is most associated with cosmetic skin maintenance via exfoliation, but can also occur biologically or for medical reasons.
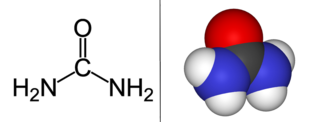
Urea, also known as carbamide-containing cream, is used as a medication and applied to the skin to treat dryness and itching such as may occur in psoriasis, dermatitis, or ichthyosis. It may also be used to soften nails.
The intense contact between a musical instrument and skin may exaggerate existing skin conditions or cause new skin conditions. Skin conditions like hyperhidrosis, lichen planus, psoriasis, eczema, and urticaria may be caused in instrumental musicians due to occupational exposure and stress. Allergic contact dermatitis and irritant contact dermatitis are the most common skin conditions seen in string musicians.
Topical drug delivery (TDD) is a route of drug administration that allows the topical formulation to be delivered across the skin upon application, hence producing a localized effect to treat skin disorders like eczema. The formulation of topical drugs can be classified into corticosteroids, antibiotics, antiseptics, and anti-fungal. The mechanism of topical delivery includes the diffusion and metabolism of drugs in the skin. Historically, topical route was the first route of medication used to deliver drugs in humans in ancient Egyptian and Babylonian in 3000 BCE. In these ancient cities, topical medications like ointments and potions were used on the skin. The delivery of topical drugs needs to pass through multiple skin layers and undergo pharmacokinetics, hence factor like dermal diseases minimize the bioavailability of the topical drugs. The wide use of topical drugs leads to the advancement in topical drug delivery. These advancements are used to enhance the delivery of topical medications to the skin by using chemical and physical agents. For chemical agents, carriers like liposomes and nanotechnologies are used to enhance the absorption of topical drugs. On the other hand, physical agents, like micro-needles is other approach for enhancement ofabsorption. Besides using carriers, other factors such as pH, lipophilicity, and drug molecule size govern the effectiveness of topical formulation.
References
- ↑ Kaneko F, Itoh N, Yoshida H, Suzuki M, Ono I (December 1991). "The cell-components and cytokines in the subcorneal microabscess of psoriasis". Fukushima J Med Sci. 37 (2): 103–12. PMID 1823882.
- ↑ "DermPathTutor©-Munro Microabscess". Archived from the original on 2009-03-26. Retrieved 2009-03-02.
- ↑ Braun-Falco, Otto (2000-09-27). Dermatology. p. 489. ISBN 978-3540166726.
- ↑ Steffen C (August 2002). "William John Munro and Munro's abscess, and Franz Kogoj and Kogoj's spongiform pustule". Am J Dermatopathol. 24 (4): 364–8. doi:10.1097/00000372-200208000-00016. PMID 12142621.
- ↑ Johnson, A. 1983. The Man behind the Eponym. William John Munro (1863–1908). The American Journal of Dermatopathology 5(5): 477–478.