Related Research Articles

Retinopathy is any damage to the retina of the eyes, which may cause vision impairment. Retinopathy often refers to retinal vascular disease, or damage to the retina caused by abnormal blood flow. Age-related macular degeneration is technically included under the umbrella term retinopathy but is often discussed as a separate entity. Retinopathy, or retinal vascular disease, can be broadly categorized into proliferative and non-proliferative types. Frequently, retinopathy is an ocular manifestation of systemic disease as seen in diabetes or hypertension. Diabetes is the most common cause of retinopathy in the U.S. as of 2008. Diabetic retinopathy is the leading cause of blindness in working-aged people. It accounts for about 5% of blindness worldwide and is designated a priority eye disease by the World Health Organization.
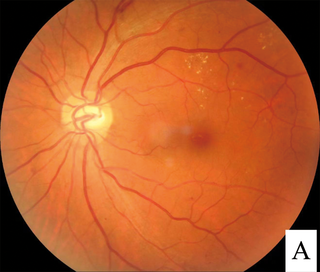
Diabetic retinopathy, is a medical condition in which damage occurs to the retina due to diabetes mellitus. It is a leading cause of blindness in developed countries.
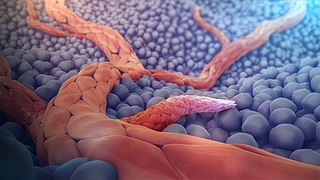
Angiogenesis is the physiological process through which new blood vessels form from pre-existing vessels, formed in the earlier stage of vasculogenesis. Angiogenesis continues the growth of the vasculature mainly by processes of sprouting and splitting, but processes such as coalescent angiogenesis, vessel elongation and vessel cooption also play a role. Vasculogenesis is the embryonic formation of endothelial cells from mesoderm cell precursors, and from neovascularization, although discussions are not always precise. The first vessels in the developing embryo form through vasculogenesis, after which angiogenesis is responsible for most, if not all, blood vessel growth during development and in disease.
This is a partial list of human eye diseases and disorders.
Vascular endothelial growth factor, originally known as vascular permeability factor (VPF), is a signal protein produced by many cells that stimulates the formation of blood vessels. To be specific, VEGF is a sub-family of growth factors, the platelet-derived growth factor family of cystine-knot growth factors. They are important signaling proteins involved in both vasculogenesis and angiogenesis.
Vasculogenesis is the process of blood vessel formation, occurring by a de novo production of endothelial cells. It is sometimes paired with angiogenesis, as the first stage of the formation of the vascular network, closely followed by angiogenesis.
Rubeosis iridis is a medical condition of the iris of the eye in which new abnormal blood vessels are found on the surface of the iris.
Therapeutic angiogenesis is an experimental area in the treatment of ischemia, the condition associated with decrease in blood supply to certain organs, tissues, or body parts. This is usually caused by constriction or obstruction of the blood vessels. Angiogenesis is the natural healing process by which new blood vessels are formed to supply the organ or part in deficit with oxygen-rich blood. The goal of therapeutic angiogenesis is to stimulate the creation of new blood vessels in ischemic organs, tissues, or parts with the hope of increasing the level of oxygen-rich blood reaching these areas.

Presumed ocular histoplasmosis syndrome (POHS) is a syndrome affecting the eye, which is characterized by peripheral atrophic chorioretinal scars, atrophy or scarring adjacent to the optic disc and maculopathy.
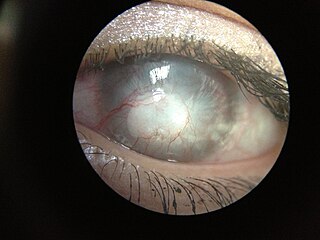
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of corneal pathophysiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.
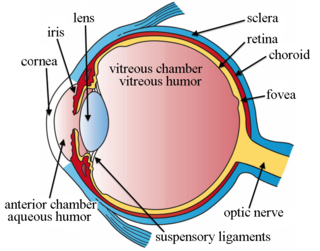
Choroidal neovascularization (CNV) is the creation of new blood vessels in the choroid layer of the eye. Choroidal neovascularization is a common cause of neovascular degenerative maculopathy commonly exacerbated by extreme myopia, malignant myopic degeneration, or age-related developments.

Pigment epithelium-derived factor (PEDF) also known as serpin F1 (SERPINF1), is a multifunctional secreted protein that has anti-angiogenic, anti-tumorigenic, and neurotrophic functions. Found in vertebrates, this 50 kDa protein is being researched as a therapeutic candidate for treatment of such conditions as choroidal neovascularization, heart disease, and cancer. In humans, pigment epithelium-derived factor is encoded by the SERPINF1 gene.

Vascular endothelial growth factor A (VEGF-A) is a protein that in humans is encoded by the VEGFA gene.

Intraocular hemorrhage is bleeding inside the eye. Bleeding can occur from any structure of the eye where there is vasculature or blood flow, including the anterior chamber, vitreous cavity, retina, choroid, suprachoroidal space, or optic disc.
Retinal gene therapy holds a promise in treating different forms of non-inherited and inherited blindness.

Familial exudative vitreoretinopathy is a genetic disorder affecting the growth and development of blood vessels in the retina of the eye. This disease can lead to visual impairment and sometimes complete blindness in one or both eyes. FEVR is characterized by incomplete vascularization of the peripheral retina. This can lead to the growth of new blood vessels which are prone to leakage and hemorrhage and can cause retinal folds, tears, and detachments. Treatment involves laser photocoagulation of the avascular portions of the retina to reduce new blood vessel growth and risk of complications including leakage of retinal blood vessels and retinal detachments.

Radiation retinopathy is damage to retina due to exposure to ionizing radiation. Radiation retinopathy has a delayed onset, typically after months or years of radiation, and is slowly progressive. In general, radiation retinopathy is seen around 18 months after treatment with external-beam radiation and with brachytherapy. The time of onset of radiation retinopathy is between 6 months to 3 years.
Aganirsen is a 25 mer DNA antisense oligonucleotide therapeutic inhibiting insulin receptor substrate-1 (IRS-1), which is being investigated as a topical treatment for ocular neovascularization. Aganirsen is a candidate for the treatment of ocular neovascularization in patients with front of the eye (cornea) or back of the eye (retinal) diseases, including progressive corneal neovascularization in patients with infectious keratitis and wet age related macular degeneration (AMD).
Joan Whitten Miller is a Canadian-American ophthalmologist and scientist who has made notable contributions to the treatment and understanding of eye disorders. She is credited for developing photodynamic therapy (PDT) with verteporfin (Visudyne), the first pharmacologic therapy for retinal disease. She also co-discovered the role of vascular endothelial growth factor (VEGF) in eye disease and demonstrated the therapeutic potential of VEGF inhibitors, forming the scientific basis of anti-VEGF therapy for age-related macular degeneration (AMD), diabetic retinopathy, and related conditions.
Sickle cell retinopathy can be defined as retinal changes due to blood vessel damage in the eye of a person with a background of sickle cell disease. It can likely progress to loss of vision in late stages due to vitreous hemorrhage or retinal detachment. Sickle cell disease is a structural red blood cell disorder leading to consequences in multiple systems. It is characterized by chronic red blood cell destruction, vascular injury, and tissue ischemia causing damage to the brain, eyes, heart, lungs, kidneys, spleen, and musculoskeletal system.
References
- ↑ Neely, Kimberly A.; Gardner, Thomas W. (1998-09-01). "Ocular Neovascularization". The American Journal of Pathology. 153 (3): 665–670. doi:10.1016/S0002-9440(10)65607-6. ISSN 0002-9440. PMC 1852998 . PMID 9736014.
- 1 2 3 4 Marín-García, José (2007). "11: Cardiac Neovascularization: Angiogenesis, Arteriogenesis, and Vasculogensis". Post-Genomic Cardiology (1 ed.). Academic Press. doi:10.1016/B978-0-12-373698-7.X5000-1. ISBN 978-0-12-373698-7.
- ↑ Dudley, A.C. & Griffioen, A.W., Pathological angiogenesis: mechanisms and therapeutic strategies. Angiogenesis, 2023. doi: 10.1007/s10456-023-09876-7
- ↑ Chiang, Homer H.; Hemmati, Houman D. (October 2013). Scott, Ingrid U.; Fekrat, Sharon (eds.). "Treatment of Corneal Neovascularization". EyeNet Magazine. American Academy of Ophthalmology: 35–6. Retrieved 14 July 2020.
- 1 2 3 Neely, Kimberly A.; Gardner, Thomas W. (September 1998). "Ocular Neovascularization: Clarifying Complex Interactions". The American Journal of Pathology. Elsevier Inc. 153 (3): 665–670. doi:10.1016/S0002-9440(10)65607-6. PMC 1852998 . PMID 9736014 . Retrieved 14 July 2020.
- ↑ Reddy U, Krzystolik M (2006). "Antiangiogenic therapy with interferon alfa for neovascular age-related macular degeneration". Cochrane Database Syst Rev (1): CD005138. doi:10.1002/14651858.CD005138.pub2. PMID 16437522.
- ↑ "Cardiovascular diseases (CVDs)". World Health Organization. 17 May 2017. Retrieved 14 July 2020.
- ↑ Lassaletta, Antonio D.; Chu, Louis M.; Sellke, Frank W. (November 2011). "Therapeutic neovascularization for coronary disease: current state and future prospects". Basic Research in Cardiology. 106 (6): 897–909. doi:10.1007/s00395-011-0200-1. PMID 21713563. S2CID 28038901.
- ↑ Johnson, Takerra; Zhao, Lina; Manuel, Gygeria; Taylor, Herman; Liu, Dong (7 February 2019). "Approaches to therapeutic angiogenesis for ischemic heart disease". Journal of Molecular Medicine. 97 (2): 141–151. doi:10.1007/s00109-018-1729-3. PMC 6417498 . PMID 30554258.